SCI论文(www.lunwensci.com):
摘要:目的讨论结直肠癌术前淋巴结转移与患者术前临床病理参数及血清肿瘤标志物的相关性。方法搜集陕西省人民医院2014年1月至2019年5月695例结直肠癌患者临床资料,纳入标准:(1)术前内镜取检,活检结果确诊CRC;(2)完整切除肿瘤并且标本进行术后病理活检;(3)患者病历及研究相关资料完整;(4)排除术前行辅助治疗者;(5)排除血液系统及其他原发肿瘤者。收集患者术前临床病理参数及血清肿瘤标志物。收集患者术后切除组织淋巴结转移信息,对数据行回顾性研究分析,选择c2检验进行单因素分析,选择Logistics多因素回归模型对淋巴结转移的高危因素进行分析。结果单因素分析结果提示患者年龄,性别,吸烟史,酗酒史,高血压史,糖尿病史,Hb,Alb与CRC淋巴结转移无相关(P>0.05)。术前肠梗阻,肿瘤组织类型,肿瘤分化程度,CEA、CA199与淋巴结转移相关(P<0.05)。对有统计学意义的高危因素进行多因素回归分析,术前肠梗阻,肿瘤分化程度,CEA与淋巴结转移相关(P<0.05)。结论术前肠梗阻,肿瘤分化程度,CEA是淋巴结转移的独立高危因素。
关键词:结直肠癌;淋巴结转移;临床病理参数;肿瘤标志物
本文引用格式:曹立强,杨国军,刘思达,等.结直肠癌术前淋巴结转移相关危险因素分析[J].世界最新医学信息文摘,2019,19(99):25-26,29.
Analysis of Risk Factors Associated with Lymph Node Metastasis in Colorectal Cancer
CAO Li-qiang1,YANG Guo-jun1,LIU Si-da1,LIU Deng-feng1,DUAN Jiang-long2*
(1.Xian Medical College,Xi'an Shaanxi;2.Shaanxi people's Hospital,Xi'an Shaanxi)
ABSTRACT:Objective To investigate the correlation between preoperative lymph node metastasis of colorectal cancer and preoperative clinical pathological parameters and serum tumor markers.Methods The clinical data of 695 patients with colorectal cancer from January 2014 to May 1919 in Shaanxi Provincial People's Hospital were collected.The criteria were included:(1)preoperative endoscopic examination,biopsy results confirmed CRC;(2)complete resection of tumor and Specimens were subjected to postoperative pathological biopsy;(3)patient medical records and related data were complete;(4)exclusion of preoperative adjuvant therapy;(5)exclusion of the blood system and other primary tumors.The preoperative clinical pathological parameters and serum tumor markers were collected.The patient's postoperative specimens were collected for lymph node metastasis.The data were analysis.The logistic multivariate regression model was used to analyze the risk factors of lymph node metastasis.Results Univariate analysis showed that patients were not associated with age,gender,smoking history,alcohol history,hypertension history,diabetes history,Hb,Alb and CRC lymph node metastasis(P>0.05).Preoperative intestinal obstruction,tumor tissue type,tumor differentiation,CEA,CA199 were associated with lymph node metastasis(P<0.05).Multivariate regression analysis of high-risk factors with statistical significance,preoperative intestinal obstruction,tumor differentiation,CEA and lymph node metastasis were associated(P<0.05).Conclusion Preoperative intestinal obstruction,tumor differentiation and CEA are independent risk factors for lymph node metastasis.
KEY WORDS:Colorectal cancer;Lymph node metastasis;Clinical pathological parameters;Serum tumor markers
0引言
结直肠癌(colorectal cancer,CRC)在国内消化道恶性肿瘤中发病率位于首位[1],并且相比世界其他地区增长迅速[2]。手术切除癌变组织仍是治疗CRC的主要方式。CRC转移的主要路径为淋巴结转移,对患者术后5年生存率有重要影响[3-4]。如果术前通过临床病理参数及术前血清肿瘤标志物及影像学检查诊断出CRC患者无淋巴结转移,在手术中,保证安全性及根治性的原则上,可以尽可能保留其功能性。术前对CRC患者进行淋巴结转移的评估,可以选择对患者获益更大的诊疗策略。目前术前检测CRC是否有淋巴结转移的金标准是淋巴结探查+病理活检,但这种方法常带来一些负面影响[5]。传统CT,MRI对CRC淋巴结转移的诊断仍有缺陷[6-7]。磁共振淋巴结造影(magnetic resonance lymphography,MRL)技术对术前CRC淋巴结检测具有明显优势[8],但其对于技术人员操作水平要求较高,无法达到普及。本研究对结直肠癌患者术前临床病理参数及血清肿瘤标志物分析,探讨CRC淋巴结转移的高危因素。
1资料与方法
1.1研究对象
对陕西省人民医院2014年1月至2019年5月695例结直肠癌患者临床病理参数及患者术前血清肿瘤标志物进行统计分析。纳入标准:(1)术前内镜取检,活检结果确诊CRC;(2)完整切除肿瘤并且标本进行术后病理活检;(3)患者病历及与研究相关资料完整;(4)排除术前行辅助治疗者;(5)排除血液系统及其他原发肿瘤者。其中淋巴结转移率为46.4%。收集患者年龄,性别,吸烟史,酗酒史,高血压史,糖尿病史,肿瘤组织类型,术前是否肠梗阻,术前Hb,术前Alb,肿瘤分化程度,术前血清CEA、CA199。
1.2方法
1.2.1手术方法
直肠癌患者均参考全直肠系膜切除(TME)的手术原则。手术方式选择经腹会阴联合切除根治术(Miles手术)或者经腹直肠癌前侧切除根治术(Dixon手术)。结肠癌患者常规切除肿瘤及相关肠系膜,清扫血管及肠系膜根部淋巴结,实施肠管吻合,反复冲洗腹腔,逐层关腹。术中远端切除距肿瘤边缘大于2cm,术中冰冻提示两端肠管无残留癌组织。
1.2.2病理学检查
肿瘤切除后用甲醛固定液固定24h,石蜡包埋后切片4微米左右并行HE染色,所有染色过的切片由两名高资历病理科医师采用双盲法分别读片,如发现淋巴结中有癌细胞浸润则定义为有淋巴结侵犯。
1.3统计方法
数据分析选择SPSS 18.0统计软件,数据用2检验,数据相关性采用pearson法,选择logistics模型对数据进行多因素分析。P<0.05有统计学意义。
2结果
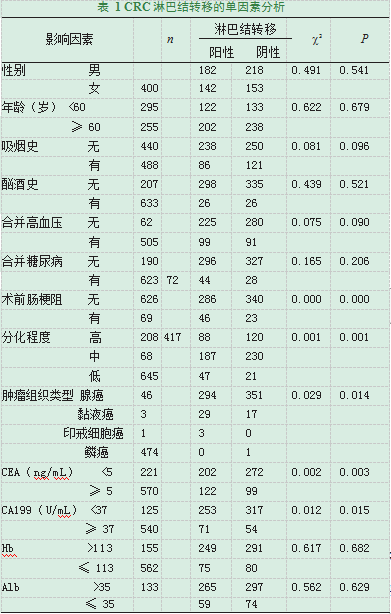
2.1术前临床病理参数及术前血清肿瘤标志物与淋巴结转移的单因素分析
患者年龄,性别,吸烟史,酗酒史,高血压史,糖尿病史,Hb,Alb与术前淋巴结转移无相关(P>0.05)。术前肠梗阻,肿瘤组织类型,肿瘤分化程度,CEA,CA199与术前淋巴结转移相关(P<0.05)(表1)。
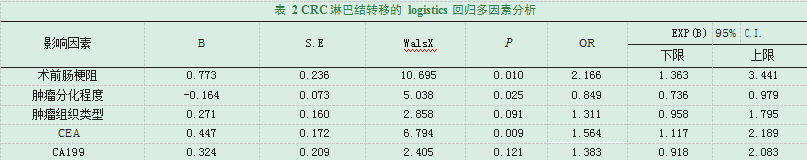
2.2淋巴结转移相关危险因素的多因素分析
对表1有统计学意义的术前临床病理参数及术前血清肿瘤标志物行多因素分析。结果提示术前肠梗阻,肿瘤分化程度,CEA对于CRC淋巴结转移有重要意义(表2)。
3讨论
CRC患者由于肿瘤增长向肠腔膨出,导致肠腔狭窄,出现梗阻症状,在左半结肠癌中较多见。肠梗阻导致肠腔局部压力上升,挤压组织液逆向流动,携带肿瘤细胞侵袭淋巴管[9]。并且由于管腔狭窄,肠内容物通过时对肿瘤反复挤压,导致肿瘤细胞浸润。当CRC患者出现梗阻症状时,往往分期较晚,肿瘤侵入肠壁较深。有研究显示,在结直肠粘膜层不存在淋巴管,在肿瘤穿透粘膜层后,淋巴管的数量逐渐增多[10-11]。因此,术前肠梗阻增加了CRC淋巴结转移风险。分化低的肿瘤细胞因其生物学特性,具有较高的侵袭性,可以早期侵袭粘膜下层及肌层,促使淋巴结转移[12]。CEA是内胚层分化而来的肿瘤细胞产生的一种肿瘤相关抗原,在正常胚胎的消化系统中也可出现,正常组织中几乎不存在[13-14]。本次研究发现,术前血清CEA阳性对CRC患者术前淋巴结转移有重要影响。在本次研究中,多因素回归分析显示肿瘤组织类型不是术前淋巴结转移的独立危险因素。但是肿瘤组织类型是印戒细胞癌的患者均发生淋巴结转移。结果可能与印戒细胞癌例数过少有关。
在右半结肠癌手术中,CME(全结肠系膜切除)的安全性及手术适应症仍备受争论,CME要求切除完整的肠系膜以及在根部结扎回结肠动静脉等血管。日本《大肠癌诊疗规约》[15]中规定,术前或者术中发现患者有淋巴结转移或肿瘤侵及肌层则应行D3淋巴结清扫。无论CME还是D3淋巴结清扫相比传统右半结肠癌手术都可以切除更多的淋巴结。但是在骨骼化回结肠静脉至Henle干之间的肠系膜上静脉时一旦损伤,处理不当将会给患者带来生命危险。而有研究显示,CME的5年生存率以及无病生存率对于传统的结肠癌手术并未体现出明显的优势[16]。因此,外科医生在术前对右半结肠癌患者进行淋巴结转移的评估,有助于选择最佳的手术方式。
20世纪初,Miles首次发现直肠癌的淋巴扩散有三个方向:向上、向外侧和向下。他强调了周围区域淋巴结在直肠癌根治术中的重要性。几项回顾性研究表明,侧方淋巴转移对直肠癌的5年生存率有重要意义[17-21]。TME的手术原则在直肠癌手术中少有争论。但是TME并不包括清扫侧方淋巴结。常规清扫侧方淋巴结会导致手术时间延长,术中出血量增加等并发症,这些因素对侧方淋巴清扫适应症提出新的要求。日本直肠癌侧方淋巴结清扫手术适应证为:低位直肠癌、浸润深度T3以及T4、肠系膜内有淋巴结转移[21]。因此,术前筛选出有淋巴结转移的患者,在保证TME的原则上有选择性的实施侧方淋巴结清扫可以更好的把握手术适应症,使手术更加标准及精细化。直肠癌手术已经趋于规范,但是否切除左结肠动脉的问题仍无定论。理论上肠系膜下动脉的高位结扎能够拥有更好的肠管活动度,同时使淋巴结清扫彻底,但有研究显示肠系膜下动脉高位结扎与低位结扎在术后5年生存率无显著差异[22]。也有学者指出低位结扎可以降低直肠癌根治术后吻合口瘘的风险[23],但目前尚无荟萃分析及随机对照研究证实高位结扎使吻合口瘘的概率增加。因此,是否行肠系膜下动脉高位结扎还看术者习惯,但是如果术前明确肿瘤侵犯肠系膜血管根部淋巴结,则应高位结扎肠系膜下动脉。
综上所述,术前肠梗阻,肿瘤分化程度,以及CEA是淋巴结转移的重要危险因素,对有淋巴结转移高危因素的患者可以联合影像学检查,如MRL技术,实现对CRC患者淋巴结转移评估的精确化,从而制定对患者获益最大的诊疗策略。
参考文献
[1]Bray F,Ferlay J,Soerjomataram I,et al.Global cancer statistics 2018:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J].CA:a cancer journal for clinicians,2018,68(6):394-424.
[2]RyanÉ,Khaw YL,Creavin B,et al.Tumor Budding and PDC Grade Are Stage Independent Predictors of Clinical Outcome in Mismatch Repair Deficient Colorectal Cancer[J].The American journal of surgical pathology,2018,42(1):60-68.
[3]Resch A.Lymph node staging in colorectal cancer:old controversies and recent advances[J].World journal of gastroenterology,2013,19(46):8515-8526.
[4]Edge SB.The American Joint Committee on Cancer:the 7th edition of the AJCC cancer staging manual and the future of TNM[J].Annals of surgical oncology,2010,17(6):1471-1474.
[5]Hahn HS,Song HS,Lee IH,et al.Magnetic resonance imaging and intraoperative frozen sectioning for the evaluation of risk factors associated with lymph node metastasis in endometrial cancer[J].International journal of gynecological cancer:official journal of the International Gynecological Cancer Society,2013,23(8):1411-1416.
[6]Heijnen LA,Lambregts DM,Mondal D,et al.Diffusion-weighted MR imaging in primary rectal cancer staging demonstrates but does not characterise lymph nodes[J].European radiology,2013,23(12):3354-3360.
[7]刘栋,宋斌,孙学军,等.FTIR结合主成分分析法对直肠癌转移淋巴结的研究[J].光谱学与光谱分析,2017,37(07):2028-2031.
[8]Fortuin AS,Deserno WM,Meijer HJ,et al.Value of PET/CT and MR lymphography in treatment of prostate cancer patients with lymph node metastases[J].International journal of radiation oncology,biology,physics,2012,84(3):712-718.
[9]Baxter LT.Transport of fluid and macromolecules in tumors I Role of interstitial pressure and convection[J].Microvascular research,1989,37(1):77-104.
[10]Ding PR,An X,Cao Y,et al.Depth of tumor invasion independently predicts lymph node metastasis in T2 rectal cancer[J].Journal of gastrointestinal surgery:official journal of the Society for Surgery of the Alimentary Tract,2011,15(1):130-136.
[11]Li H,Lu P,Lu Y,et al.Predictive factors of lymph node metastasis in undifferentiated early gastric cancers and application of endoscopic mucosal resection[J].Surgical oncology,2010,19(4):221-226.
[12]Matsumoto Y,Saito M,Saito K,et al.Enhanced expression of KIF4A in colorectal cancer is associated with lymph node metastasis[J].Oncology letters,2018,15(2):2188-2194.
[13]TrapéJ,Filella X,Alsina-Donadeu M,et al.Increased plasma concentrations of tumour markers in the absence of neoplasia[J].Clinical chemistry and laboratory medicine,2011,49(10):1605-1620.
[14]Sisik A,Kaya M,Bas G,et al.CEA and CA 19-9 are still valuable markers for the prognosis of colorectal and gastric cancer patients[J].Asian Pacific journal of cancer prevention:APJCP,2013,14(7):4289-4294.
[15]Neeff HP,Drognitz O,Klock A,et al.Impact of preoperative targeted therapy on postoperative complications after resection of colorectal liver metastases[J].International journal of colorectal disease,2012,27(5):635-645.
[16]Killeen S,Mannion M,Devaney A.Complete mesocolic resection and extended lymphadenectomy for colon cancer:a systematic review[J].Colorectal disease:the official journal of the Association of Coloproctology of Great Britain and Ireland,2014,16(8):577-594.
[17]Moriya Y,Sugihara K,Akasu T.Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer[J].World journal of surgery,1997,21(7):728-732.
[18]Morita T,Murata A,Koyama M,et al.Current status of autonomic nerve-preserving surgery for mid and lower rectal cancers:Japanese experience with lateral node dissection[J].Diseases of the colon and rectum,2003,46(10 Suppl):S78-87;discussion S87-8.
[19]Sato H,Maeda K,Maruta M,et al.Who can get the beneficial effect from lateral lymph node dissection for Dukes C rectal carcinoma below the peritoneal reflection?[J].Diseases of the colon and rectum,2006,49(10 Suppl):S3-12.
[20]Ueno H,Mochizuki H,Hashiguchi Y,et al.Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection[J].Annals of surgery,2007,245(1):80-87.
[21]Sugihara K,Kobayashi H,Kato T,et al.Indication and benefit of pelvic sidewall dissection for rectal cancer[J].Diseases of the colon and rectum,2006,49(11):1663-1672.
[22]Yang Y,Wang G,He J,et al.High tie versus low tie of the inferior mesenteric artery in colorectal cancer:A meta-analysis[J].International journal of surgery(London,England),2018,52():20-24.
[23]Zang L,Ma J.Effect of preserving left colic artery during radical operation of rectal cancer on anastomotic leakage and operation time[J].Zhonghua wei chang wai ke za zhi=Chinese journal of gastrointestinal surgery,2016,19(4):386-387.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网! 文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/22652.html