SCI论文(www.lunwensci.com):
摘要:目的探讨不同术后镇痛方案对老年人行胸腔镜下肺叶切除术后苏醒期躁动及术后早期认知功能影响观察。方法将2017年11月至2018年11月在我院胸外科行胸腔镜下肺叶切除术的90例老年患者按不同术后镇痛方案分为三组,A组采用全身麻醉复合硬膜外麻醉术后静脉镇痛,B组采用全身麻醉复合硬膜外麻醉术后硬膜外镇痛,C组采用全凭静脉麻醉术后静脉镇痛,比较三组的术后苏醒质量、躁动及认知功能。结果两组T1时Riker镇静-躁动评分无明显差异(P>0.05),A组和B组T2、T3、T4、T5时Riker镇静-躁动评分明显低于C组(P<0.05);A组和B组术后1 d的POCD发生率明显低于C组(P<0.05),而三组在术后3 d、7 d的POCD发生率无明显差异(P>0.05)。结论全身麻醉复合硬膜外麻醉术后硬膜外镇痛对老年人行胸腔镜下肺叶切除术后苏醒速度快,苏醒质量高,发生躁动几率低,认知功能影响小,可优先选择。
关键词:胸腔镜下肺叶切除术;老年人;不同术后镇痛方案;术后躁动;术后早期认知功能
本文引用格式:吴越,王婷婷,刘岩松,等.不同术后镇痛方案对老年人行胸腔镜下肺叶切除术后苏醒期躁动及术后早期认知功能影响观察[J].世界最新医学信息文摘,2019,19(64):8-9.
Observation of the Effects of Different Postoperative Analgesia Regimens on Emergence Agitation and Early Postoperative Cognitive Function on Elderly Patients Treated with Thoracoscopic Lobectomy
WU Yue1,WANG Ting-ting1,LIU Yan-song1,ZHENG Qiu-yu2*
(1.Department of Anesthesiology,The First Affiliated Hospital of Dalian Medical University,Dalian,Liaoning,116000;2.Department of Cardiology,Jilin Hospital of Integrated Traditional Chinese and Western Medicine,Changchun,Jilin,132500)
ABSTRACT:Objective To explore the effects of different postoperative analgesia regimens on emergence agitation and early postoperative cognitive function on elderly patients treated with thoracoscopic lobectomy.Methods 90 elderly patients who received thoracoscopic lobectomy in the department of thoracic surgery in the First Affiliated Hospital of Dalian Medical University from November 2017 to November 2018 were selected for study.They were divided into three groups named Group A,Group B,and Group C respectively according to different postoperative analgesia schemes.General anesthesia combined with epidural anesthesia as well as postoperative intravenous analgesia were adopted in Group A.General anesthesia combined with epidural anesthesia as well as postoperative epidural analgesia were provided in Group B.Only intravenous anesthesia and postoperative intravenous analgesia were used in Group C.The quality of postoperative recovery,agitation and cognitive function of the patients were compared among the three groups.Results At T1,there was no significant difference in Riker sedation-agitation scores among the three groups(P>0.05).Riker sedation-agitation scores of the patients in group A and group B at T2,T3,T4 and T5 were significantly lower than those in group C(P<0.05).The incidence of POCD of the patients in group A and group B was significantly lower than that in group C(P<0.05),while there was no significant difference in the incidence of POCD at 3 days and 7 days after surgery among the three groups(P>0.05).Conclusion The implication of general anesthesia combined with epidural anesthesia as well as postoperative epidural analgesia in the recovery of elderly patients treated with thoracoscopic lobectomy enjoy rapid recovery speed,high recovery quality,low incidence of agitation,and relatively little effect on cognitive function.Therefore,it may take priority.
KEY WORDS:Thoracoscopic lobectomy;Elderly patient;Different postoperative analgesia schemes;Postoperative agitation;Early postoperative cognitive function
0 引言
胸腔镜下肺叶切除术是治疗肺癌的主要方法,通过切除肿瘤原发病灶和转移病灶,减轻机体肿瘤负荷,但手术时麻醉方法的选择至关重要,手术麻醉及术后镇痛会影响老年患者的脑血流供应,导致术后苏醒期发生躁动、认知功能障碍(POCD),影响患者的术后恢复[1]。因此,选择合理的手术麻醉及术后镇痛方案至关重要。本研究进一步分析不同术后镇痛方案对老年人行胸腔镜下肺叶切除术后苏醒期躁动及POCD的影响,现具体汇报如下。
1资料与方法
1.1一般资料。将2017年11月至2018年11月在我院胸外科行胸腔镜下肺叶切除术的90例老年患者按不同术后镇痛方案分为三组。A组30例,男13例,女17例,年龄62-80岁,平均(68.6±5.4)岁;B组30例,男14例,女16例,年龄61-79岁,平均(68.1±5.6)岁;C组30例,男17例,女13例,年龄61-80岁,平均(68.7±5.9)岁;所有患者均符合胸腔镜下肺叶切除术手术标准,ASA分级在Ⅰ-Ⅱ级;排除术前合并POCD、精神系统及神经系统疾病;比较三组间的年龄、性别、手术方法及ASA分级无明显差异,具有可比性。
1.2方法。所有患者术前30 min肌注阿托品0.5 mg,入室后连接心电监护。C组采用全凭静脉麻醉,麻醉诱导使用咪达唑仑0.1 mg/kg,舒芬太尼0.3µg/kg,顺式阿曲库铵0.15 mg/kg,靶控输注瑞芬太尼6 ng/mL、丙泊酚4μg/ml,之后连接双腔气管插管机械通气,麻醉维持采用靶控输注瑞芬太尼和丙泊酚,顺式阿曲库铵0.06mg/kg/h维持肌松,术毕30 min前连接自控静脉镇痛泵(PCIA),药用0.01%酒石酸布托啡诺及雷莫司琼0.6 mg,加入生理盐水100 mL中,持续镇痛,速度2 mL/h[2]。A组和B组均行T5-T6或T6-T7椎间隙行硬膜外穿刺麻醉,注入1%利多卡因5 mL测试麻醉平面,确定无全脊麻后行全身麻醉诱导,方法同C组,之后连接双腔气管插管机械通气,麻醉维持采用靶控输入丙泊酚、硬膜外泵入0.25%罗哌卡因4 mL/h、顺式阿曲库铵0.06 mg/kg/h,术毕前30 minA组连接PCIA同C组,B组连接自控硬膜外镇痛泵(PCEA),药用0.25%罗哌卡因5 mL/h[3]。三组术后均维持镇痛48 h。
1.3观察指标。采用Riker镇静-躁动评分评估术后躁动情况,分为自主呼吸恢复时(T1)、呼唤睁眼时(T2)、拔管时(T3)、拔管后10 min(T4)及拔管后30 min(T5);采用术后恢复质量评估量表(PQRS)评估术后1 d、3 d、7 d的POCD发生率。
1.4统计学分析。采用SPSS 19.0统计学软件,计数资料行χ2检验,率(%)表示,计量资料用t检验,均数±标准差(±s)表示,以P<0.05表示有统计学差异。
2结果
2.1三组间不同时间点Riker镇静-躁动评分比较,见表1。
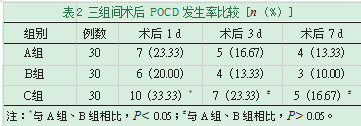
2.2三组间术后POCD发生率比较,见表2。
3讨论
麻醉苏醒期躁动及POCD均是常见麻醉并发症。躁动主要是由于术后脑组织缺血缺氧,发生炎性反应及再灌注损伤,是脑组织受损的一种外在表现形式,临床需要应用镇静药物,不仅延长了机械通气时间,也增加了并发症发生率。躁动多见于全身麻醉,硬膜外麻醉较少发生,全身麻醉可导致交感神经兴奋,血流动力学波动增大,应激反应强烈,而硬膜外麻醉能够阻滞感觉与交感神经,抑制其兴奋,降低应激反应,维持血流动力学平稳[4]。同时,硬膜外麻醉能够减少全麻药物的用量,增强抑制痛觉传导的功能,能缩短术后苏醒时间,加快自主呼吸恢复时间[5]。另外,疼痛也是诱发躁动的重要因素之一。POCD发生的危险因素较多,苏醒期躁动、长时间麻醉、高龄等均是诱发因素,一旦发病,可造成人格及行为异常,甚至影响远期生活质量[6]。本研究结果显示,A组和B组T2、T3、T4、T5时Riker镇静-躁动评分明显低于C组(P<0.05);A组和B组术后1 d的POCD发生率明显低于C组(P<0.05)。说明全身麻醉复合硬膜外麻醉及术后硬膜外镇痛发生躁动的几率最低,能有效减轻脑组织损伤。而POCD的发病与麻醉方式及术后镇痛方式的关联不大,但降低躁动发生率有助于改善认知功能。
综上所述,采用全身麻醉复合硬膜外麻醉及术后硬膜外镇痛对老年人行胸腔镜下肺叶切除术后苏醒期躁动的降低效果最好,有利于保护脑组织功能,降低POCD发生率。
参考文献
[1]马蓉.不同麻醉和镇痛方案对胸腔镜下肺癌根治术后老年患者苏醒期躁动及认知功能的影响[J].中国医学前沿杂志(电子版),2017,9(12):110-114.
[2]陈冀衡,张云宵,李萍,等.胸椎旁神经阻滞或肋间神经阻滞复合全麻对胸腔镜手术患者术后镇痛的影响[J].临床麻醉学杂志,2014,30(5):444-447.
[3]赖学文,莫惠飞,公维义,等.氟比洛芬酯复合舒芬太尼静脉镇痛与肋间神经阻滞用于胸腔镜手术的镇痛效果[J].中国医学创新,2018,15(12):103-105.
[4]刘先岭,智明明,王静静,等.胸椎旁神经阻滞复合全身麻醉对胸腔镜肺癌根治术患者镇痛及免疫细胞功能的影响[J].中国现代医学杂志,2017,27(22):47-51.
[5]廖明锋,迟晓慧,罗爱林.全身麻醉复合椎旁阻滞对肺叶切除术患者术后恢复的影响[J].临床外科杂志,2016,24(9):709-711.
[6]程少先,李海波,徐文礼,等.超声引导椎旁阻滞复合全麻对胸腔镜肺叶切除术后患者苏醒及早期恢复质量的影响[J].临床肺科杂志,2018,23(2):323-327.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网! 文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/18664.html