SCI论文(www.lunwensci.com):
摘要:目的观察养肝解郁颗粒治疗非酒精性脂肪性肝病(肝郁脾虚、内有郁热证)的临床疗效。方法选择非酒精性脂肪性肝病(肝郁脾虚、内有郁热证)患者60例,随机分为治疗组和对照组各30例。治疗组采用养肝解郁颗粒治疗,对照组口服多烯磷脂胆碱胶囊,均治疗24周。治疗前后观察两组中医证候积分、肝功能、血脂、肝/脾CT比值。结果治疗组中医证候总有效率(86.67%)显著高于对照组(73.33%)(P<0.01)。治疗组治疗后各中医症状积分均显著降低(P<0.01),对照组胁肋胀痛、脘腹胀满、倦怠乏力、便溏不爽、口干口苦症状均存在统计学差异(P<0.01),恶心嗳气、食欲不振、烦躁易怒症状存在统计学差异(P<0.05);治疗后组间比较,胁肋胀痛、脘腹胀满、便溏不爽、恶心嗳气、烦躁易怒均存在统计学差异(P<0.05),而倦怠乏力、食欲不振、口干口苦症状无统计学差异(P>0.05)。肝功能(ALT、AST、GGT)治疗前后组内比较,其结果均有统计学差异(P<0.01、P<0.05);组间比较两组无统计学差异(P>0.05)。血脂治疗前后组内比较,TG、LDL-C治疗前后两组疗效均有统计学差异(P<0.01,P<0.05),TC治疗组治疗前后有统计学差异(P<0.01),对照组治疗前后比较无统计学差异(P>0.05);治疗组治疗后效果明显优于对照组(P<0.05)。两组患者肝/脾CT比较,治疗组总有效率(86.67%)高于对照组(60.00%)(P<0.05)。结论养肝解郁颗粒治疗非酒精性脂肪性肝病(肝郁脾虚、内有郁热证)的临床疗效确切,与对照组多烯磷脂胆碱胶囊对比,在改善临床症状、降低血脂及调节肝/脾CT比值方面具有明显优势。
关键词:非酒精性脂肪性肝病;养肝解郁颗粒;多烯磷脂胆碱胶囊;临床研究
本文引用格式:杨明,矫越,冷炎.养肝解郁颗粒治疗非酒精性脂肪性肝病(肝郁脾虚、内有郁热证)的临床观察[J].世界最新医学信息文摘,2019,19(70):1-2,6.
Clinical Observation of Yanggan Jieyu Granule in the Treatment of Non-alcoholic Fatty Liver Disease(Liver Depres-sion and Spleen Deficiency,Internal Stagnation Heat Syndrome)
YANG Ming1,JIAO Yue2,LENG Yan1△
(1 Affiliated Hospital of Changchun University of Traditional Chinese Medicine,Changchun,Jilin;2 Changchun Tongyuan Hospital,Changchun,Jilin)
ABSTRACT:Objective To observe the clinical efficacy of Yanggan Jieyu Granule in the treatment of non-alcoholic fatty liver dis-ease(liver depression and spleen deficiency,internal stagnation heat syndrome).Methods 60 patients with non-alcoholic fatty liver disease(liver depression and spleen deficiency,internal stagnation of heat syndrome)were selected,they were randomly divided into treatment group and control group with 30 cases of each group.The treatment group was treated with yanggan jieyu granule,while the control group was treated with polyene phosphatidylcholine capsule,all patients were treated for 24 weeks.Before and after treatment,the scores of TCM syndromes,liver function,blood lipid and liver/spleen CT ratio were observed.Results The total effective rate of TCM syndromes in the treatment group(86.67%)was significantly higher than that in the control group(73.33%)(P<0.01).The scores of TCM symptoms in the treatment group were significantly lower(P<0.01),in the control group,there were significant differences in the symptoms of flank and rib pain,epigastric fullness,fatigue and fatigue,bad stool,dry mouth and bitter mouth(P<0.01),there were sta-tistical differences in nausea,belching,anorexia,irritability and irritability(P<0.05);After treatment,there were significant differences between the two groups in the pain of flank and rib,abdominal distention,fecal discomfort,nausea and belching,irritability and irrita-bility(P<0.05),there was no significant difference in burnout,loss of appetite,dry mouth and bitter mouth(P>0.05).The results of liver function(ALT,AST,GGT)before and after treatment were significantly different(P<0.01,P<0.05);There was no significant difference between the two groups(P>0.05).The blood lipids were compared before and after treatment,there were significant differences between the two groups before and after treatment with TG and LDL-C(P<0.01,P<0.05),the TC of the treatment group had statistical difference before and after treatment(P<0.01),while the control group had no statistical difference before and after treatment(P>0.05);The effect of treatment group was better than that of control group(P<0.05).The liver/spleen CT were compared between the two groups,the total effective rate of treatment group(86.67%)was higher than that of control group(60.00%)(P<0.05).Conclusion Yanggan jieyu granule is effective in treating non-alcoholic fatty liver disease(liver depression and spleen deficiency,internal stagnation heat syndrome),com-pared with the control group treated with polyene phosphatidylcholine capsule,it has obvious advantages in improving clinical symp-toms,reducing blood lipids and regulating the ratio of liver to spleen CT.
KEY WORDS:Non-alcoholic fatty liver disease;Yanggan jieyu granules;Polyene phosphatidylcholine capsules;Clinical research
0引言
非酒精性脂肪性肝病(non-alcoholic fatty liver disease,NA-FLD)是除外酒精及其他明确的损肝因素,以超过5%的肝脏存在脂肪堆积为主要特征的综合征,现一般认为属代谢综合征(meta-bolic syndrome,MetS)[1]的肝病部分。NAFLD全球发生率、死亡率及发病率逐年升高,其对健康的影响及所造成的经济负担也逐年增加[2]。与非酒精性脂肪性肝炎(non-alcoholic steatohepatitis,NASH)相关的肝硬化目前已成为发达国家肝移植的第二大原因,预计将成为其最常见的适应证[3]。养肝解郁颗粒为丹栀逍遥散加减化裁,采用古方制为颗粒剂。经动物实验证实本药具有减轻NAFLD肝纤维化模型鼠的肝细胞损伤程度、改善肝纤维化等功效,进而开展本临床研究,验证其有效性及安全性。
1资料与方法
1.1一般资料
60例NAFLD患者,均为2018年7月至2019年4月于长春中医药大学附属医院门诊就诊的患者。将患者随机分为治疗组(养肝解郁颗粒)和对照组(多烯磷脂胆碱胶囊),治疗组入组32例,脱落2例,其中男17例,女13例,平均年龄(41.857±10.020)岁,CT病情分级比例轻∶中∶重为7∶15∶8;对照组入组35例,脱落5例,其中男14例,女16例,平均年龄(40.500±10.342)岁,CT病情分级比例轻∶中∶重为7∶18∶5。两组间性别、年龄和病情等一般资料比较无统计学差异(P>0.05),具有可比性。
1.2纳入标准
NAFLD的临床诊断标准符合中华医学会肝病学分会脂肪肝和酒精性肝病组2010年1月修订的《非酒精性脂肪性肝病诊疗指南》。肝郁脾虚,内有郁热中医诊断标准参考2002年《中药(新药)临床研究指导原则》中病毒性肝炎及高脂血症的临床指导原则制定。全部患者均符合诊断标准,年龄在18-65周岁,2周内未服用过保肝药物及降脂、减肥药物。
1.3治疗方法
两组患者均在限制饮食热量、改善饮食组分、中等量有氧运动的基础上,治疗组给予养肝解郁颗粒(牡丹皮、栀子、当归、白芍、柴胡、茯苓、炒白术、炙甘草、生姜、薄荷、决明子组成,由本院制剂室统一制剂为颗粒剂),每次10g,每日3次,温开水冲服。对照组给予多烯磷脂胆碱胶囊,每次456mg,每日3次,口服。两组均连续治疗24周[4-6]。
1.4观察指标
1.4.1中医临床证候积分
治疗前后参考《中药(新药)临床研究指导原则》中评分标准,记录胁肋胀痛、脘腹胀满、倦怠乏力、便溏不爽、恶心嗳气、食欲不振、烦躁易怒、口干口苦症状积分和总积分。
1.4.2肝功能检测
包括血清谷氨酸氨基转移酶(alanine aminotransferase,ALT)、门冬氨酸氨基转移酶(aspartate transaminase,AST)、谷氨酰转肽酶(γ-glutamyl transpeptadase,GGT)。
1.4.3血脂检查
包括甘油三酯(triglyceride,TG)、总胆固醇(total cholesterol,TC)、低密度脂蛋白(low density lipoprotein,LDL-C)。
1.4.4肝/脾CT比值
肝/脾CT值之比<1.0。其中肝/脾CT比值<1.0但>0.7者为轻度,≤0.7但>0.5者为中度,≤0.5者为重度脂肪肝。
2结果
2.1两组患者中医证候疗效比较见表1、表2。
如表1所示:经治疗后,按照中医证候疗效判定标准,治疗组治愈5例,显效13例,有效8例,未愈4例;对照组治愈2例,显效4例,有效16例,未愈8例;治疗组治疗后总有效率明显高于对照组(P<0.01)。
如表2所示:经秩和检验,各症状治疗前评分无统计学差异。治疗组疗效确切,治疗前后各症状组内比较均存在显著统计学差异(P<0.01);对照组疗效尚可,治疗前后组内对比中,胁肋胀痛、脘腹胀满、倦怠乏力、便溏不爽、口干口苦症状均存在统计学差异(P<0.01),恶心嗳气、食欲不振、烦躁易怒症状存在统计学差异(P<0.05)。
治疗后组间比较,胁肋胀痛、脘腹胀满、便溏不爽、恶心嗳气、烦躁易怒均存在统计学差异(P<0.05),而倦怠乏力、食欲不振、口干口苦症状,两组治疗后无统计学差异(P>0.05)。
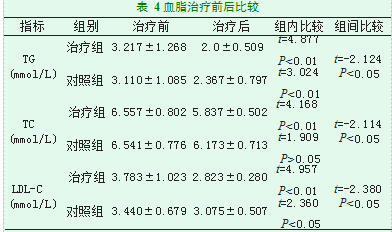
2.2两组NAFLD患者治疗前后肝功及血脂比较见表3、表4。
如表3所示,两组患者治疗后与治疗前肝功能(ALT、AST、GGT)比较,组内比较,其结果均有统计学差异(P<0.01、P<0.05);两组治疗后无统计学差异(P>0.05)。
如表4所示,血脂治疗前后组内比较,TG、LDL-C治疗前后两组疗效均有统计学差异(P<0.01、P<0.05),TC治疗组治疗前后有统计学差异(P<0.01),对照组治疗前后比较无统计学差异(P>0.05);治疗后治疗组优于对照组(P<0.05)。
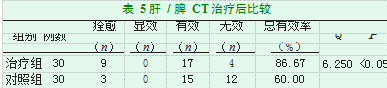
2.3两组NAFLD患者治疗后肝/脾CT比较见表5。
如表5所示,经过治疗后,两组患者肝/脾CT比较,治疗组与对照组的总有效率分别为86.67%和60.00%,结果有统计学差异(P<0.05)。
3结论
研究结果表明,养肝解郁颗粒治疗非酒精性脂肪性肝病(肝郁脾虚、内有郁热证),对于患者的临床症状有明显的改善效果,特别是针对临床常见的胁肋胀痛、脘腹胀满、便溏不爽、恶心嗳气、烦躁易怒等主要症状。养肝解郁颗粒对NAFLD患者肝功能、血脂、肝/脾CT比值均有一定的治疗作用[7-9]。与对照组多烯磷脂胆碱胶囊对比,在改善临床症状、降低血脂及调节肝/脾CT比值方面具有明显优势。
4讨论
生活干预是现代医学治疗NAFLD的基础,不仅可以改善肝脏病变,而且能改善血糖、血脂、血压,控制相关的心血管危险因素。应用维生素E、利拉鲁肽可以逆转NASH的进展,奥贝胆酸可以明显改善肝脏组织学,但其相关研究证据较少,在NAFLD治疗中的作用尚不明确,其他方法如应用他汀类药物、n-3多元不饱和脂肪酸、手术等,均能一定程度改善血脂、血糖及心血管风险,但对NAFLD并无直接治疗作用。
NAFLD归属中医“胁痛”、“肝癖”等范畴[10],曾红丽等[11]回顾性分析244例NAFLD患者中医证候及相关指标,其中肝郁脾虚证占115例(47.1%),后依次是湿热蕴结、痰浊内阻、痰瘀阻络、肝肾阴虚等证。李敏谦等[12]检索了2297篇相关文献,收录病例16796例,其中主要致病因素为湿(24.32%)、气滞(15.38%)、气虚(14.81%)和痰(14.22%),主要病位在肝(48.40%)和脾(38.85%)。中医药治疗NAFLD具有因人制宜的优势,经典方剂的对证应用更有奇效。因此,对于经典方剂制剂工艺、具体应用回顾性研究等方面,还需进一步挖掘整理。
参考文献
[1]Younossi Z M,Stepanova M,Rafiq N,et al.Pathologic criteria for nonalco-holic steatohepatitis:Interprotocol agreement and ability to predict liver-relat-ed mortality[J].Hepatology,2011,53(6):1874-1882.
[2]Younossi Z M,Koenig A B,Abdelatif D,et al.Global epidemiology of non-alcoholic fatty liver disease-Meta-analytic assessment of prevalence,incidence, and outcomes[J].Hepatology,2016,64(1):73-84.
[3]Rinella M E.Nonalcoholic Fatty Liver Disease:A Systematic Review[J].JAMA,2015,313(22):2263-2273.
[4]胡义扬.中医药治疗非酒精性脂肪性肝病的优势与展望[J].世界中医药,2015(2):149-152.
[5]李军祥.中医药治疗非酒精性脂肪性肝病专题笔谈[J].中国中西医结合消化杂志,2017(11):801-804.
[6]罗莉川,纪云西,谢利双,等.中医药治疗非酒精性脂肪性肝病的研究进展[J].按摩与康复医学,2017(24):3-6.
[7]魏功昌,何瑾瑜.中医体质辨识治疗非酒精性脂肪性肝病[J].长春中医药大学学报,2018,34(3):116-119.
[8]王洁,杨旋,乔治园,等.中医药治疗非酒精性脂肪性肝病的研究进展[J].新疆中医药,2018(2):145-147.
[9]刘三都.非酒精性脂肪性肝病的中医药治疗[J].肝博士,2017(6):57-58.
[10]孟江涛.中医药治疗非酒精性脂肪性肝炎的有效性及安全性[J].世界最新医学信息文摘,2015,15(74):15-16.
[11]曾红丽,刘军楼,汪红.非酒精性脂肪肝中医证型及相关证候的临床分析[J].环球中药,2018,11(05):685-689.
[12]李敏谦,林育,项磊,等.基于临床文献的非酒精性脂肪性肝病证候分布规律研究[J].世界中医药,2019,14(01):6-11.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网! 文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/20409.html