SCI论文(www.lunwensci.com):
摘要:目的研究老年男性在丙泊酚复纳布啡静脉麻醉下行膀胱镜检查的有效性及安全性。方法选取我院2018年5月至2019年6月择期行膀胱镜检查的老年男性患者104例,按照随机数字表法将患者分为丙泊酚复合纳布啡组(A组,实验组)和单纯丙泊酚组(B组,对照组),除外失访及中途退出者,A组51例,B组50例。A组:开始检查前缓慢注射纳布啡0.15mg/kg+丙泊酚2mg/kg;B组:单纯注射丙泊酚2mg/kg。若术中出现体动反应则追加丙泊酚,每次0.5mg/kg。采用VAS评分随访两组患者术后尿道疼痛情况,记录围术期患者心率(HR)、平均动脉压(MAP)、血氧饱和度(SpO2),观察术中两组患者体动反应、呼吸抑制情况,记录两组患者的麻醉诱导时间、膀胱镜检查时间、苏醒时间、丙泊酚用量及恶心呕吐、头晕头痛等不良反应发生情况。结果与B组相比,A组患者丙泊酚用量明显减少,差异有统计学意义(P<0.05);苏醒时间A组较B组略短,但差异无统计学意义(P>0.05);A组患者在术后小6时内VAS评分较B组低,差异有统计学意义(P<0.05);两组患者SpO2、HR、MAP与同组术前相比均有所波动,但两组间差异无统计学意义(P>0.05);A组中恶心呕吐、呼吸抑制、躁动不安、体动反应例数明显少于B组,差异有统计学意义(P<0.05)。结论纳布啡复合丙泊酚可用于老年男性患者无痛膀胱镜检查,效果优于单纯应用丙泊酚,术中血流动力学平稳,麻醉效果及术者操作满意,并可明显减轻术后副反应及尿道疼痛,是一种安全有效的麻醉方法。
关键词:无痛膀胱镜;前列腺增生;纳布啡;丙泊酚;老年男性
本文引用格式:张海航,任益锋,李会芳,等.丙泊酚复合纳布啡静脉麻醉用于老年男性膀胱镜检的临床研究[J].世界最新医学信息文摘,2019,19(98):12-15.
Clinical Study of Propofol combined with Nalbuphine Intravenous Anesthesia for Elderly Males on Painless Cystoscopy
ZHANG Hai-hang,REN Yi-feng,LI Hui-fang,CHEN Cheng-zhe,ZHENG Xiao-zhen,WANG Lian-qu*
(The First Affiliated Hospital of Henan University,Kaifeng Henan)
ABSTRACT:Objective To study the efficacy and safety of propofol combined with nalbuphine intravenous anesthesia for elderly males on painless cystoscopy.Methods 104 elderly males patients who underwent painless cystoscopy during May 2018 to June 2019 were selected and divided into two groups according to random number table method.Except the patients lost follow-up or dropped out,the group A has the number of 51 patients and group B has 50.The group A were injected with nalbuphine 0.15mg/kg and propofol 2mg/kg.The group B were injected with propofol 2mg/kg only.Propofol 0.5mg/kg were added if the body reaction occurs during the cystoscopy.Following-up of urethral pain in both groups with VAS score.The heart rate(HR),mean arterial pressure(MAP)and pulse oxygen saturation(SpO2)were compared between the two groups in the perioperative period.The numbers of body reaction and respiration inhibition were observed during the cystoscopy.Their Anesthesia induction time,operation time,recovery time,propofol dosage and side effects such as nausea,vomiting,dizziness and headache were recorded.Results Compared with the B group,the dosage of propofol in the A group was significantly reduced,with statistically difference(P<0.05).The recovery time of group A was slightly shorter than group B,but the difference was not statistically significant(P<0.05).The VAS score of patients in group A was lower than that of group B at 6 hours after operation,and the difference was statistically significant(P<0.05).The SpO2,HR,and MAP of the two groups were fluctuated compared with those of the same group before surgery,but there was no statistical significance between the two groups.The incidence of nausea and vomiting,respiratory depression,restlessness and numbers of body reaction in group A was lower than that in group B,with statistically difference(P<0.05).Conclusion Nalbuphine combine with propofol can be used for painless cystoscopy in elderly male patients.The effect is better than using propofol alone.The hemody-namics is stable during operation,the anesthetic effect and the operation of the surgeon are satisfactory,the incidence of side reaction and urinary pain can be significantly reduced.It is a safe and effective method of anesthesia on painless cystoscopy.
KEY WORDS:Painless cystoscopy;Benign prostatic hyperplasia;Nalbuphine;Propofol;Elderly males
0引言
硬性膀胱镜检查泌尿外科的重要检查手段之一,临床上多用于诊断、随访膀胱和输尿管疾病,是一项泌尿外科医生必须熟练掌握的基本检查。但由于该检查方式是一种侵入性操作,尤其对于男性病人,尿道结构较女性尿道长而复杂,在镜体通过时患者尿道时易产生胀痛不适感[1],加之行膀胱镜检查患者多为老年男性,前列腺增生在60~80岁男性中发病率高达50~83%[2],增生的前列腺组织在术中操作镜体时会受到镜体的压迫,使绝大多数患者感到疼痛难忍和恐惧感,部分患者出现尿道括约肌痉挛和膀胱颈收缩[3],使患者难以配合,加之老年患者常伴有基础疾病,可诱发恶心呕吐、心脑血管意外[4,5]。传统的全麻镇痛方式采用单纯静脉应用丙泊酚[1,6],尤其对于前列腺增生患者镇痛效果不佳、术后副反应大。纳布啡是一种具有呼吸抑制作用弱、镇痛效应强、血流动力学平稳、且成瘾性低的镇痛药物[7],常与丙泊酚联合应用于短小手术的麻醉,目前尚无纳布啡用于老年男性无痛膀胱镜检查的临床研究。因此,我们旨通过设计这项随机、双盲对照研究,从而进一步确定其安全性和有效性。
1资料与方法
1.1临床资料
选取我院泌尿外科2018年5月至2019年6月择期行膀胱镜检查的老年男性患者,所有患者术前均行彩超检查明确前列腺大小,前列腺体积计算公式为0.52×前后径×左右径×上下径[8],计算结果体积≥60mL认定为大体积前列腺,体积<60mL认定为小体积前列腺[9]。本研究共招募患者104人,采用随机数字表法将患者分为丙泊酚复合纳布啡组(A组)和单纯丙泊酚组(B组),研究期间A组有1例患者中途退出,B组有2例患者失访,最终共纳入101例患者,其中A组51例,B组50例。该研究方案经伦理学委员会批准,所有患者均知情同意并签署知情同意书。
(1)纳入标准:①所有经影像学检查不能明确诊断的膀胱或输尿管疾病的老年男性患者(≥60岁);怀疑膀胱或尿道病变或需取活体组织进行病理检查者;②需确定血尿的原因及出血部位,确定尿频、排尿困难原因的患者;③入选患者均符合美国麻醉医师协会分级(ASA)Ⅰ~Ⅲ级,且Mallampati气道分级Ⅰ~Ⅱ级;④所有患者术前查肝肾功能、心肺功能未见明显手术禁忌,既往无内分泌疾病、神经及精神系统疾病,近期未服药抗凝药物。
(2)排除标准:①泌尿生殖器官处于急性炎症期不宜进行检查的患者;②急性全身感染性疾病、出血性疾病、病情严重患者;③膀胱容量小于50mL以下者;④包茎、严重尿道狭窄、尿道内结石嵌顿等无法插入膀胱镜者;⑤骨关节畸形不宜采取截石体位者。
1.2麻醉方法
所有患者术前6小时禁食、4小时禁饮,入室后连接监护仪测量患者平均动脉压(MAP)、血氧饱和度(SpO2)、心率(HR),开放静脉通路并用鼻导管吸氧2~3min后,A组患者缓慢注射盐酸纳布啡(后简称纳布啡;宜昌人福药业有限公司,批号:1180202)0.15mg/kg,时间60s,随后注射丙泊酚注射液(后简称丙泊酚;四川国瑞药业有限责任公司,批号:1809101)2mg/kg,待患者睫毛反射消失后行膀胱镜检,如患者出现体动反应,则追加丙泊酚0.5mg/kg。B组患者单纯注射丙泊酚2mg/kg,待患者睫毛反射消失后行膀胱镜检,如患者出现体动反应,则追加丙泊酚0.5mg/kg。同时检测两组患者生命体征,若心率降至60次/分以下,则静脉注射阿托品0.01mg/kg。若血压降低较基础值30%,则给予麻黄碱0.1mg/kg,若患者SpO2降至90%以下,则采取仰额抬颏或面罩给氧。检查结束后停药,待患者生命体征平稳,意识恢复后离开。
1.3膀胱镜检查方法
嘱患者术前排空膀胱,清醒下取截石位,常规消毒铺巾,石蜡油润滑尿道口及膀胱镜镜体,待麻醉达成后使用WOLF F22 5°膀胱镜直视下进入尿道,缓慢沿尿道前壁推至尿道前列腺部,待尿道括约肌松弛后适当下压镜体,以顺利进入膀胱,膀胱颈明显抬高时可适当增加下压幅度,通过膀胱镜将生理盐水灌入膀胱,使膀胱适当充盈,观察膀胱三角区及膀胱颈口,保留膀胱镜外鞘,更换70°膀胱内镜,适当旋转、摇摆镜体依次观察双侧输尿管口、膀胱后壁、侧壁、顶壁、前壁,检查完毕后排空膀胱,更换5°膀胱内镜后直视下退出镜体。
1.4观察指标
采用视觉模拟评分法(VAS)随访两组患者术后2小时、4小时、6小时、12小时的尿道疼痛情况,在一个10cm的标尺上左端标记为0分右端标记为10分,0分表示无痛,3分以下表示有轻微的疼痛,但尚能忍受,4~6分表示疼痛并影响睡眠,尚能忍受,7~10分表示无法忍受的疼痛。记录患者麻醉前5min(T0)、麻醉后(T1)、检查结束后(T2)、麻醉苏醒(T3)后MAP、SpO2、HR。记录两组患者的膀胱镜检查时间、麻醉诱导时间、苏醒时间、丙泊酚用量、术中体动反应、呼吸抑制、躁动不安情况以及术后恶心呕吐、头晕嗜睡等不良反应发生情况。
1.5样本量计算
本研究类型为随机对照试验,结局指标为术后4 h的VAS评分,属于定量变量,根据前期预试验,实验组的VAS评分均值为2.3,对照组为3.7,检验水准α=0.05,把握度1-β为90%,采用G*Power 1.3.7.软件进行样本量计算,得出每组样本量为48,考虑到可能有10%的患者存在中途退出或失访等情况,最终决定每组纳入患者的样本量为52人。
1.6统计学分析
采用SPSS 24.0统计软件进行数据分析,计量资料以均数±标准差(x±s)表示,组内比较采用重复测量的方差分析,组间比较采用两独立样本t检验进行分析;计数资料以百分比(%)表示,采用卡方检验。所有统计分析均使用双侧检验,P<0.05代表差异具有统计学意义。
2结果
2.1两组患者一般资料比较
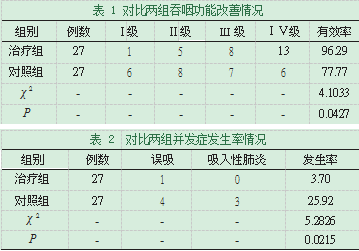
本研究中A组的丙泊酚平均用量为(75.51±10.76)mg,明显比对照组的(126.53±14.18)mg少,组间差异具有统计学意义(P<0.05),苏醒时间A组较B组略短,但差异无统计学意义(P>0.05),年龄、体重、麻醉诱导时间、膀胱镜检时间等指标两组间差异无统计学意义(P<0.05),见表1。
2.2两组患者术后尿道疼痛随访
A组患者在术后2小时、4小时、6小时内的VAS评分低于B组患者,差异有统计学意义(P<0.05);两组术后12小时患者仍有轻微疼痛症状,疼痛程度均呈减轻趋势,但VAS评分组间对比无明显差异(P>0.05),见表2。
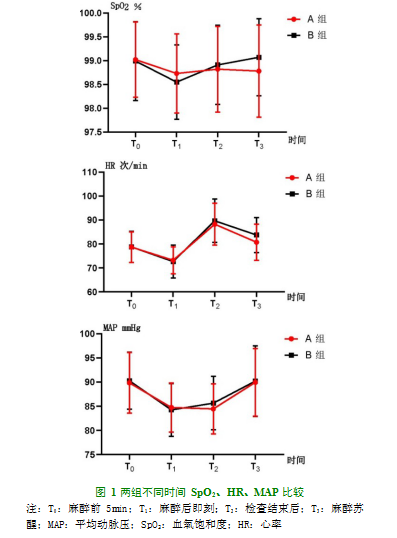
2.3两组不同时间SpO2、HR、MAP比较
与同组T0相比,两组T1~T3时SpO2、HR、MAP均有所波动,其中对照组HR与MAP波动较大,但组间比较差异无统计学意义(P>0.05),见图1。
2.4两组不良反应发生率
A组恶心呕吐、呼吸抑制、躁动不安、体动反应发生率较B组低,差异有统计学意义(P<0.05);与B组相比,A组嗜睡、头晕发生率略低,但差异无统计学意义(P>0.05),见表3。
3讨论
随着社会人口老龄化的发展,尿频、尿急、尿痛、肉眼血尿等下尿路症状在老年人群中发病率逐渐升高[10],当前的B超及多排螺旋CT检查的分辨率虽然大大提高,但是对于直径约1~5 mm的膀胱占位及原位癌仍难以被发现[11],有文献报道一组浸润性膀胱癌患者行CT检查,诊断准确率只有54.9%,39%分期偏低[12]。通过膀胱镜检查可以明确膀胱内有无肿瘤、膀胱粘膜异常、以及膀胱结石等疾病,必要时可以对病变部位行活检,因此膀胱镜检和活检是诊断膀胱肿瘤、下尿路症状原因以及膀胱癌术后随访最可靠的办法[13]。膀胱镜检查是通过人体自然尿道进镜,男性尿道长约18~22cm,在非勃起状态下呈“S”型,且进镜过程中需要经过生理弯曲及狭窄,镜检过程中男性患者有明显的胀痛不适感[14],尤其对于前列腺增生患者,镜体在经过后尿道膜部时需下压镜体以通过上抬的前列腺后唇,会产生明显的疼痛不适感[15]。Stav等人应用疼痛评分法发现,患者在膀胱镜检前存在着明显的恐惧和焦虑[14],从而引起患者配合不佳,影响检查效果。无痛膀胱镜检查是指在做膀胱镜检查前,先对患者实施静脉麻醉,减轻患者检查时的痛苦。
老年患者无痛膀胱镜检的麻醉重点在于保证术中呼吸、循环系统的稳定,丙泊酚因其起效时间快、苏醒时间短、无蓄积效应广泛应用于无痛膀胱镜、肠镜等检查[16,17],但因其镇痛作用较弱,在膀胱镜检过程中进镜、下压、旋转、摇摆镜体时,增生的前列腺体受到压迫[18],患者因疼痛产生体动反应,发生迷走神经反射,使得尿道括约肌收缩,加大进镜难度[19],单独应用丙泊酚时往往需大剂量才能满足手术要求,随剂量增加对循环、呼吸系统的抑制也会增加[20]。有报道显示[21],静推丙泊酚2.5-3.0mg/kg后,血压降幅可达19.5%-25.0%。本研究中2例患者血压降低超过麻醉前50%,9例患者降低超过麻醉前20%-30%,8例患者在静脉注射丙泊酚后出现呼吸抑制,分别给予麻黄素、面罩通气后上述情况好转。因而丙泊酚需联合对呼吸、循环系统较轻微的镇痛药物,减少其用量,降低不良反应,并减少因疼痛引起的刺激。
纳布啡是一种κ受体激动μ受体拮抗剂阿片类药物,其镇痛强度类似于吗啡,可同时发挥拮抗和激动的双重作用,具有封顶效应,呼吸抑制、心血管不良反应发率较低,和舒芬太尼等阿片类药物相比,血流动力学更平稳,纳布啡起效迅速,静脉注射3分钟后可发挥镇痛效果,镇痛效果可维持3~6小时,术毕仍具有一定的镇痛效果[22]。本研究中使用丙泊酚复合纳布啡,在术后6小时内患者VAS评分明显低于对照组,并且丙泊酚使用量、心率、平均动脉压、血氧饱和度的波动均小于对照组,术后不良反应、尿道疼痛发生率较对照组明显降低。
同时,我们还观察到,体动反应多发生在镜体通过后尿道时,尤其对于大体积前列腺患者该反应生更加明显,这可能因前列腺增生致使膀胱颈后唇抬高,因而需要大幅度下压镜体以通过后尿道,该操作会压迫前列腺引起疼痛[23,24],可诱发或加重前列腺充血,这也是术后患者尿道疼痛的主要原因,因而本研究认为,对于大体积前列腺患者,可适当追加纳布啡用量。
老年患者约50%左右合并有心血管系统疾病,在全麻下行膀胱镜检存在一定程度的风险,加之老年人呼吸功能减退,应用全麻药物时应尽量避免影响其血流动力学及呼吸抑制。本研究显示,丙泊酚复合纳布啡静脉全麻能够在能够达到手术要求的前提下,较单独应用丙泊酚,能够明显减少丙泊酚用量,从而减轻老年人循环和呼吸抑制,减少术中因疼痛发生的体动反应,有利于术者操作,避免尿道损伤,且术后尿道疼痛症状有明显改善,恶心呕吐等不良反应发生率降低,因而本研究认为丙泊酚复合纳布啡可安全有效地用于老年患者的无痛膀胱镜检查中。
参考文献
[1]Poletajew S,Bender S,Pudełko P,et al.Anaesthesia of the posterior urethra and pain reduction during cystoscopy-a randomized controlled trial[J].Wideochirurgia i inne techniki maloinwazyjne=Videosurgery and other miniinvasive techniques,2017,12(1):75-80.
[2]Gu FL,Xia TL,Kong XT.Preliminary study of the frequency of benign pros-tatic hyperplasia and prostatic cancer in China[J].Urology,1994,44(5):688-91.
[3]Sarkar D,Kapoor K,Pal DK.Pain and anxiety assessment during cystoureth-roscopy in males using voiding instruction:A prospective,randomized con-trolled study[J].Urology annals,2018,11(2):139-42.
[4]Fazelifar A,Eskandari A,Hashemi M,et al.Deep sedation in patients under-going atrioventricular nodal reentry tachycardia ablation[J].Research in car-diovascular medicine,2013,2(4):176-9.
[5]Liu Y,Li M,Yang D,et al.Closed-loop control better than open-loop control of profofol TCI guided by BIS:a randomized,controlled,multicenter clinical trial to evaluate the CONCERT-CL closed-loop system[J].PloS one,2015,10(4):e0123862.
[6]信文启,李爱香,闫增.不同麻醉方法用于膀胱镜检查术的效果[J].中华麻醉学杂志,2015,35(6):767-8.
[7]张振,罗辉宇,徐阳,等.丙泊酚分别复合盐酸纳布啡、地佐辛、舒芬太尼用于无痛胃镜的效果比较[J].中国药房,2017,28(03):315-8.
[8]Homma Y,Gotoh M,Kawauchi A,et al.Clinical guidelines for male lower urinary tract symptoms and benign prostatic hyperplasia[J].International journal of urology:official journal of the Japanese Urological Association,2017,24(10):716-29.
[9]Roehrborn CG,McConnell JD,Lieber M,et al.Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia.PLESS Study Group[J].Urology,1999,53(3):473-80.
[10]Malde S,Patel A,Martínez-Piñeiro L,et al.Incidence of Nocturia in Men with Lower Urinary Tract Symptoms Associated with Benign Prostatic Enlarge-ment and Outcomes After Medical Treatment:Results from the Evolution European Association of Urology Research Foundation Prospective Multina-tional Registry[J].European urology focus,2019.
[11]Yang T,Li Y,Li J,et al.Diagnostic Value Comparison of Urothelium Carcinoma Among Urine Exfoliated Cells Fluorescent In Situ Hybridization(FISH)Examination,Computerized Tomography(CT)Scan,and Urine Cytologic Examination[J].Medical science monitor:international medical journal of experimental and clinical research,2018,24(5):88-92.
[12]Paik ML,Scolieri MJ,Brown SL,et al.Limitations of computerized tomography in staging invasive bladder cancer before radical cystectomy[J].The Journal of urology,2000,163(6):1693-6.
[13]Humphrey PA,Moch H,Cubilla AL,et al.The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part B:Prostate and Bladder Tumours[J].European urology,2016,70(1):106-19.
[14]Stav K,Leibovici D,Goren E,et al.Adverse effects of cystoscopy and its impact on patients'quality of life and sexual performance[J].The Israel Med-ical Association journal:IMAJ,2004,6(8):474-8.
[15]Taghizadeh AK,Madani A,El,Gard PR,et al.When does it hurt?Pain during flexible cystoscopy in men[J].Urologia Internationalis,2006,76(4):301-3.
[16]Li DN,Zhao GQ,Su ZB.Propofol Target-controlled Infusion in Anesthesia Induction during Painless Gastroscopy[J].Journal of the College of Physi-cians and Surgeons--Pakistan:JCPSP,2019,29(7):604-7.
[17]Deng C,Wang X,Zhu Q,et al.Comparison of nalbuphine and sufentanil for colonoscopy:A randomized controlled trial[J].PloS one,2017,12(12):e0188901.
[18]Palit V,Ashurst HN,Biyani CS,et al.Is using lignocaine gel prior to flexible cystoscopy justified?A randomized prospective study[J].Urol Int,2003,71(4):389-92.
[19]Kim JH,Jeen YM,Song YS.Ectopic prostate tissue at the bladder dome pre-senting as a bladder tumor[J].The world journal of men's health,2013,31(2):176-8.
[20]Burmeister MA,Brauer P,Wintruff M,et al.A comparison of anaesthetic techniques for shock wave lithotripsy:the use of a remifentanil infusion alone compared to intermittent fentanyl boluses combined with a low dose propo-fol infusion[J].Anaesthesia,2002,57(9):877-81.
[21]Agrawal M,Asthana V,Sharma JP.Efficacy of intravenous midazolam versus clonidine as premedicants on bispectral index guided propofol induction of anesthesia in laparoscopic cholecystectomy:A randomized control trial[J].Anesthesia Essays&Researches,2014,8(3):302-6.
[22]詹锐,张晓琴,杨梅,等.纳布啡复合丙泊酚用于无痛人流术[J].临床麻醉学杂志,2018,34(08):816-7.
[23]Yerlikaya G,Laml T,Elenskaia K,et al.Pain perception during outpatient cystoscopy:a prospective controlled study[J].European journal of obste-trics,gynecology,and reproductive biology,2014,173(10):1-5.
[24]Krajewski W,Kościelska-Kasprzak K,Rymaszewska J,et al.How different cystoscopy methods influence patient sexual satisfaction,anxiety,and depres-sion levels:a randomized prospective trial[J].Quality of life research:an in-ternational journal of quality of life aspects of treatment,care and rehabilita-tion,2017,26(3):625-34.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网! 文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/25496.html