SCI论文(www.lunwensci.com):
摘要:皮肤鳞状细胞癌(cutaneous squamous cell carcinoma,cSCC)是最常见的转移性非黑色素瘤,其发病率随着年龄的增长和日晒时长的增加而增加。微环境中持续的炎症是促进cSCC发展的一个明确的诱因。探究与肿瘤发生相关的慢性炎症模式有助于识别新的靶分子并指导临床治疗。
关键词:皮肤鳞状细胞癌;炎性体;免疫细胞;炎性通路
本文引用格式:王雅洁,孙乐栋.炎症在皮肤鳞状细胞癌发生发展中的作用[J].世界最新医学信息文摘,2019,19(95):35-36+38.
Effect of Inflammation in Development of CSCC
WANG Ya-jie,SUN Le-dong(Corresponding Author)
(Dermatology Department,Southern Medical University Zhujiang Hospital,Guangzhou Guangdong 510280)
ABSTRACT:Cutaneous squamous cell carcinoma(CSCC)is the most common metastatic non melanoma,with increasing incidence along with age and sun exposure time.Persistent inflammation under microenvironment is clear inducement to promote development of CSCC.Exploring chronic inflammatory patterns associated with tumorigenesis can help identify new targets and guide clinical treatment.
KEY WORDS:Cutaneous squamous cell carcinoma;Inflammasome;Immunocyte;Inflammatory pathway
0引言
皮肤鳞状细胞癌(cutaneous squamous cell carcinoma,cSCC)是最常见的转移性非黑色素瘤,近40年其发病率呈上升趋势且在较年轻的年龄组中呈发展趋势,是值得警惕的公共卫生问题[1]。慢性炎症微环境的维持促进了cSCC的发生、侵袭和转移[2]。在此我们讨论了炎症在cSCC发生发展中的作用机制,以加深对其作为发病诱因及治疗方向的认知。
1炎性体
炎症体是参与炎症发生的先天免疫反应的重要组成部分,其作为外源性和内源性危险信号的传感器被触发激活后分泌促炎细胞因子白介素-1β(IL-1β)和IL-18[3]。炎性体是由细胞质传感器、分子凋亡相关斑点样蛋白(ASC)和半胱氨酸天冬氨酸蛋白酶1前体(pro-caspase-1)组成的复合体,其中传感器包括核苷酸结合寡聚化结构域(NOD)样受体1(NLRP1)、NLRP3及黑色素瘤缺乏因子2(AIM2)等[4]。长短波紫外线对皮肤造成直接损伤,导致活性氧生成和DNA的损伤,从而激活炎性体[5]。炎症体激活在不同肿瘤的发生发展中的作用有所出入。研究表明,AIM2在皮肤鳞状细胞癌中的表达显著高于正常皮肤组织,而AIM2基因敲除可导致cSCC细胞活性降低并开始凋亡[6]。此外,AIM2基因敲除可减少侵袭性蛋白酶MMP1、MMP13的产生从而降低了cSCC细胞的侵袭性并抑制了体内cSCC的生长及血管化[6]。而ASC则通过启动子特异性甲基化在去分化cSCC中表达沉默[7]。Sand等人的研究进一步证明NLRP1炎性体组分(NLRP1、ASC、caspase-1及proIL-1β)在cSCC细胞系中的表达因甲基化而沉默,研究表明此炎性体组分的下调导致了肿瘤细胞凋亡的抑制,进而有利于皮肤肿瘤的晚期发展[8]。
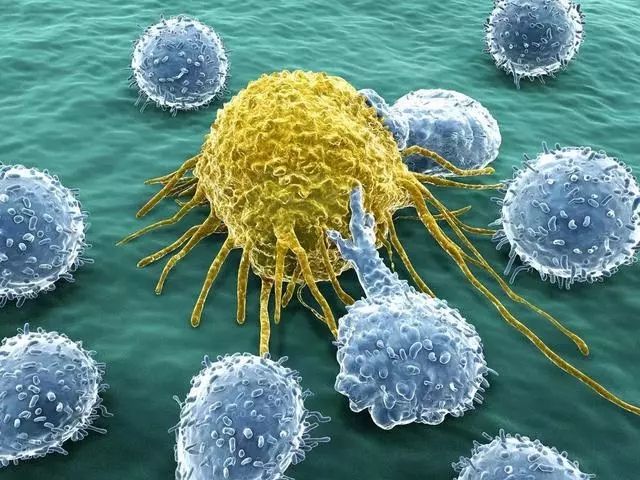
2免疫细胞及相关细胞因子
越来越多的证据表明慢性炎症参与了肿瘤的发生发展[9]。慢性炎症主要通过2型辅助性T细胞(Th2)及调节性T细胞分泌促肿瘤细胞因子(如IL-4、IL-6、IL-10、转化生长因子-β(TGF-β)等)[10]。与Th2相关的多种先天免疫细胞如巨噬细胞、肥大细胞和嗜酸性粒细胞的聚集亦可促进肿瘤的发展,其中肥大细胞和嗜酸性粒细胞是细胞外基质调节剂,可介导组织破坏并支持肿瘤的生长[11]。cSCC的炎性反应强于基底细胞癌,且低分化cSCC的炎性细胞浸润强于高分化cSCC[12]。浸润在cSCC细胞间的T细胞、巨噬细胞和肥大细胞通过与肿瘤细胞直接接触进行相互作用[12]。免疫组化证明了cSCC瘤周浸润着大量IL-17+和IL-22+T细胞[13]。体外培养cSCC细胞系,IL-17和IL-22能促进肿瘤细胞的增殖及迁移。IL-17单独或者与TNF-α联合可诱导IL-6、IL-8的产生,且IL-17和IL-22可分别激活NF-κB和STAT3通路[13]。Dibra等人在皮肤中发现了一类新的促肿瘤炎性细胞—内皮素A受体(Endothelin A receptor,ETAR)阳性CD11b细胞[14]。IL-27通过增加皮肤中ETAR阳性CD11b细胞的浸润促进了癌前炎性微环境的形成,进而导致皮肤癌变。在cSCC患者中,患者肿瘤基质中IL-27RA阳性细胞的数量与cSCC的去分化程度呈正相关关系[14]。此外,研究表明肿瘤周围细胞毒性的CD8+T细胞分布数量较多的cSCC患者有较长的生存期且其肿瘤细胞的增殖指数更低[15]。
3炎性通路
NF-κB是调控应激反应、细胞凋亡及免疫功能的重要信号通路,上皮组织中NF-κB的特异性缺失可引起肿瘤形成和严重的炎症性皮炎[16-17]。Kirkley等培育的IKK2(激活NF-κB的必需激酶)缺失的小鼠模型中部分形成了自发性cSCC。进一步的研究表明cSCC的发展不仅与表达GFAP的角质形成细胞的IKK2意外缺失有关,且与皮损中TNF的表达增加有关[18]。Toll样受体4(TLR4)信号已被证实可以驱动皮肤炎症、光免疫抑制和化学致癌[19]。Janda等发现正常皮肤向光化性角化病及cSCC进展的过程中,角质形成细胞中TLR4的表达量显著增多。使用药物拮抗TLR4可以抑制角质形成细胞和小鼠皮肤模型中由紫外线所诱导的NF-κB和激活蛋白-1(AP-1)的激活及细胞因子(IL-6、IL-8、IL-10)的分泌[20]。cSCC中HRAS、KRAS和EGFR突变的发现提示了EGFR和ERK1/2信号通路在cSCC发展过程中的重要作用[21-22]。TGF-β/p21/Nrf2通路与cSCC耐药性的产生有着密切的关系[23]。TGF-β转录激活p21及Nrf2,从而显著增强谷胱甘肽代谢并降低抗癌治疗的有效性[23]。
4 其他
研究表明组织损伤、炎症及随后的皮肤细胞外间质重塑是cSCC的启动因素,而组织学分析证实了细菌定植与cSCC的不良预后相关[24]。隐性营养不良性表皮溶解水疱症因慢性伤口的持续存在导致了cSCC,且其皮损处TGF-β1高表达、纤维形成增加导致了基质僵硬,从而形成了利于cSCC发展的微环境[25]。紫外线诱发皮肤炎症进而导致皮肤癌变是研究的热点,皮肤维生素D内分泌系统可能在此过程中发挥重要的作用[26]。荟萃分析表明维生素D受体基因多态性与cSCC发病风险相关,其中具有rs2228570、rs927650和rs1544410隐性基因型的人群患SCC的风险较低[27]。肽酰基精氨酸脱亚氨酶(peptidylargine deiminase,PAD)家族的表达及活性失调通过影响炎症反应与一系列疾病相关,过度表达PAD2的小鼠皮肤模型中诱发了自发性cSCC病变,且皮损处核磷酸化STAT3增加并有大量的炎性细胞浸润[28]。半乳糖凝集素家族在皮肤的免疫细胞和结构细胞中均可表达,其可参与调节皮肤癌症已被证实。细胞核半乳糖凝集素-3表达减少和细胞质免疫活性降低可能是促进cSCC侵袭的因素之一[29]。
炎症反应贯穿着cSCC发生发展的所有阶段。cSCC肿瘤周围炎症反应的分布及强度十分多样,提示炎性反应与肿瘤之间的复杂作用关系。探究与肿瘤发生相关的慢性炎症模式有助于识别新的靶分子并指导临床治疗。
参考文献
[1]Kim I Y,He Y Y.Ultraviolet radiation-induced non-melanoma skin cancer:Regulation of DNA damage repair and inflammation[J].Genes&Diseases,2014,1(2):188-198.
[2]Nissinen L,Farshchian M,Riihil?P,et al.New perspectives on role of tumor microenvironment in progression of cutaneous squamous cell carcinoma[J].Cell and Tissue Research,2016,365(3):691-702.
[3]Strowig,T.,et al.,Inflammasomes in health and disease[J].Nature,2012,481(7381):278-286.
[4]Feldmeyer L,Keller M,Niklaus G,等.The Inflammasome Mediates UVB-Induced Activation and Secretion of Interleukin-1βby Keratinocy tes[J].Current Biology,2007,17(13):1140-1145.
[5]Farshchian M,Nissinen L,Siljamäki E,et al.Tumor cell-specific AIM2 regulates growth and invasion of cutaneous squamous cell carcinoma[J].Oncotarget,2017,8(28):45825-45836.
[6]Meier K,Drexler S K,Eberle F C,et al.Silencing of ASC in Cutaneous Squamous Cell Carcinoma[J].Plos One,2016,11(10):e0164742.
[7] M Qin,A Pirouz,MH Kim,等.Propionibacterium acnes induces IL-1βsecretion via the NLRP3 inflammasome in human monocytes[J].Journal of Investigative Dermatolo gy,2014,134(2):381-388.
[8]Lin W W,Karin M.A cytokine-mediated link between innate immunity,inflammation,and cancer[J].Journal of Clinical Inv estigation,2007,117(5):1175-1183.
[9]Yu S H,Bordeaux J S,Baron E D.The immune system and skin c ancer[J].Oxygen Transport to Tis sue XXXIII,2014,810(810):182-191.
[10]Golomb L,Sagiv A,Pateras I S,et al.Age-associated inflammation connects RAS-induced senescence to stem cell dysfunction and epidermal malignancy[J].Cell Death and Differentiation,2015.
[11]Avrămoiu I,Petrescu I O,Ciurea M E,et al.Peritumoral
inflammatory reaction in non-melanoma skin cancers-histological and immunohistochemical study[J].Romanian journal of morphology and embryology=Revue roumaine de morphologie et embryologie,2016,57(3):943.
[12]Nardinocchi L,Sonego G,Passarelli F,et al.Interleukin-17 and interleukin-22 promote tumor progression in human nonmelanoma skin cancer[J].European Journal of Immunology,2015,45(3):922-931.
[13]Dibra D,Mitra A,Newman M,et al.IL27 controls skin tumorigenesis via accumulation of ETAR-positive CD11b cells in the pre-malignant skin[J].Oncotarg et,2016,7(47):77138-77151.
[14]Zancope E,Costa N L,Junqueirakipnis A P,et al.Differential infiltration of CD8+and NK cells in lip and oral cavity squamous cell carcinoma.[J].Journal of Oral Pathology&Medicine,2010,39(2):162-167.
[15]Wullaert A,Bonnet M C,Pasparakis M.NF-|[kappa]|B in the regulation of epithelial homeostasis and inflammation[J].Cell Research,2011,21(1):168-178.
[16]Sun X F,Zhang H.NFKB and NFKBI polymorphisms in relation to susceptibility of tumour and other diseases[J].Histology&Histopathology,2009,22(12):1387-98.
[17]Kirkley K S,Walton K D,Duncan C,et al.Spontaneous Development of Cutaneous Squamous Cell Carcinoma in Mice with Cell-specific Deletion of Inhibitor ofκB Kinase 2[J].Comp Med,2017,67(5):407-415.
[18]Wesley L,Eva S,Hui L,et al.Regulation of ultraviolet radiation induced cutaneous photoimmunosuppression by Toll-like receptor-4[J].Archives of Biochemistry&Biophysics,2011,508(2):171-177.
[19]Janda J,Burkett N B,Blohm-Mangone K,et al.Resatorvid-based Pharmacological Antagonism of Cutaneous TLR4 Blocks UV-induced NF-κB and AP-1 Signaling in Keratinocytes and Mouse Skin[J].Photochemistry&Photobiology,2017,92(6):816.
[20]Ratushny V,Gober M D,Hick R,et al.From keratinocyte to cancer:the pathogenesis and modeling of cutaneous squamous cell carcinoma[J].Journal of Clinical Investigati on,2012,122(2):464-72.
[21]Boukamp P.Non-melanoma skin cancer:what drives tumor development and progression?[J].Carcinogenes is,2005,26(10):1657-1667.
[22]O shim ori N,O ristian D,Fuch s E.TG F-βprom otes heterogeneity and drug resistance in squamous cell carcinoma[J].Cell,2015,160(5):963-976.
[23]Föll M C,Fahrner M,Gretzmeier C,et al.Identification of tissue damage,extracellular matrix remodeling and bacterial challenge as common mechanisms associated with high-risk cutaneous squamous cell carcinomas[J].Matrix Biology,2017,(66):9450-9453.
[24]Guerra,L.,et al.,Stromal microenvironment in type VII collagen-deficient skin:The ground for squamous cell carcinoma development[J].Matrix Biol,2017(63):1-10.
[25]Bikle,D.D.,Vitamin D metabolism,mechanism of action,and clinical applications[J].Chem Biol,2014,21(3):319-329.
[26]VON Schuckmann,L.A.,et al.,Vitamin D Pathway Gene Polymorphisms and Keratinocyte Cancers:A Nested Case-Control Study and Meta-Analysis[J].Anticancer Res,2016,36(5):2145-2152.
[27]Mohanan,S.,et al.,PAD2 overexpression in transgenic mice augments malignancy and tumor-associated inflammation in chemically initiated skin tumors[J].Cell Tissue Res,2017,370(2):275-283.
[28]Kapucuoglu,N.,et al.,Immunohistochemical galectin-3 expression in non-melanoma skin cancers[J].Pathol Res Pract,2009,205(2):97-103.
[29]Wu,N.L.and F.T.Liu,The expression and function of galectins in skin physiology and pathology[J].Exp Dermatol,2018,27(3):217-226.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网! 文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/25001.html