SCI论文(www.lunwensci.com):
摘要:结肠息肉是消化系统常见疾病被视为结肠癌癌前病变,内镜下息肉切除作为常规治疗术后存在较高复发率。研究表明结肠息肉复发与息肉病理类型、大小、数目、内镜手术方式等因素相关。提高对结肠息肉切除术后复发因素的认识,对于制定术后个体化随访指南、降低结肠癌发病率具有重要意义。本文结合近几年最新研究进展将结肠息肉复发相关因素总结作一综述。
关键词:结肠息肉;复发因素;研究进展
本文引用格式:陈月,汪元浚.结肠息肉切除术后复发相关因素研究进展[J].世界最新医学信息文摘,2019,19(66):125-126,128.
Advances in the Study of Relapsing Factors after Colonic Polypectomy
CHEN Yue,WANG Yuan-jun*
(Graduate School of QingHai University,Xining Qinghai)
ABSTRACT:Colon polyps is one of a common diseases in the digestive system,which is considered as precancerous lesions of colon cancer.Endoscopic polypectomy as a routine treatment still has a high recurrence rate.Related researchers show that the recurrence of colon polyps were related to the pathological types,size,numbers and the types of endoscopic surgery for polyps.It has a great significance to improve the awareness of the factors about the polyp recurrence which is valuable for the development of postoperative individualized follow-up guidelines and the reduction of the incidence of colon cancer.In this review,the factors related to the recurrence of colonic polyps were reviewed.
KEY WORDS:Colonic polyp;Recurrence factors;Research progress
0引言
结肠息肉作为消化道常见病、多发病因其具有癌变可能而被广泛关注,目前内镜下结肠息肉切除的普遍开展成为预防结肠癌并降低其死亡率的有利工具[1-3]。然而结肠息肉切除术后仍存在息肉复发和癌变可能,有研究表明结肠息肉术后3-5年内复发率约占3.9%-48.3%[3-5]。目前内镜下息肉切除术后建议定期复查肠镜[6-7]。揭示内镜下结肠息肉复发的相关因素有助于制定个体化的随访时间及监测方案,本文归纳总结国内外关于有关结肠息肉复发相关因素归纳如下。
1镜检病理类型
根据结肠息肉病理组织学检查结果可分为:炎性息肉、增生性息肉、管状腺瘤、绒毛状腺瘤、锯齿状息肉等,研究认为,管状腺瘤、绒毛状腺瘤、锯齿状息肉、重度上皮内瘤变等具有高级别组织学类型的息肉复发的独立危险因素[8,9]。绒毛组织>10mm或合并高度发育不良的病理组织学类型的息肉称为晚期腺瘤,晚期腺瘤与非晚期腺瘤相比复发风险更高(P<0.05)[7,10-11]。
2大小
息肉大小为息肉复发的危险因素[8,12-13]。有研究认为,腺瘤性息肉大于40mm为复发的独立危险因素[12,13]。目前认为,息肉大小是影响息肉切除残存组织最重要因素之一,直径>20mm的腺瘤性息肉中约有4.3%-36.7%存在残留组织[9,12,14],息肉不完全切除与复发风险独立相关(P=0.002)[5]。
3数目
息肉数目影响结肠息肉的复发[4,6,15-16]。Hui Won等[15]研究认为息肉数目≧3个为复发的独立危险因素(P=0.047);Jasper L.A等[16]认为5个以上非晚期小腺瘤晚期瘤变风险大于3个或4个小腺瘤者。
4部位
有学者认为[17]近端结肠(包含升结肠、结肠肝曲、横结肠、结肠脾曲)的息肉为复发独立危险因素(P<0.05);一些学者研究认为[18],近端结肠腺瘤性息肉进展为高危组息肉的风险性高,比值比OR 1.73(95%CI,1.61-1.97)。
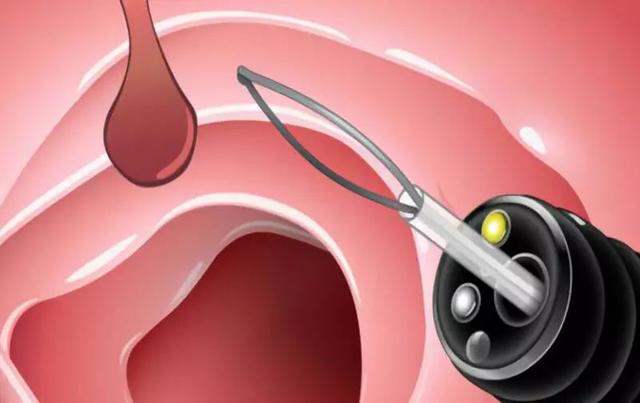
5内镜下切除方式
内镜下息肉粘膜切除术(endoscopic mucosal resection,EMR)是结肠息肉公认的治疗标准,EMR要求结肠息肉的直径在15-20mm[19]。对于直径大于2cm广基病灶通常采用内镜下分段粘膜切除术(endoscopic piecemeal mucosal resection,EPMR),EPMR是局部复发的危险因素,大息肉采用EPMR可能造成病变的不完全切除[8,20,21],切除碎片的数目与复发独立相关(P<0.05)[5,9,12]。内镜下粘膜剥离术(Endoscopic submucosal dissection,ESD)被公认为高危病变的最佳内镜下切除方式。ESD相对于EMR完全切除率高、局部复发率降低(P<0.01)[13,22,23],但由于ESD存在技术要求高、操作时间长、成本高等局限性[23-24],日本结肠息肉ESD/EMR指南建议ESD适用于晚期发育不良、早癌、术后复发等方面且具有重要价值[25]。水下内镜息肉粘膜切除术(Underwater endoscopic mucosal resection,UEMR)是一种切除大型结肠息肉的新技术。UEMR是完全切除的独立预测因子[26-27]。Robert J等[26]研究认为UEMR相对于EMR的完全切除率更高(P=0.012)、复发率低(P=0.008)、不良事件发生率无显著差异(P=0.102);Kim等[27]认为UEMR完全切除率明显高于EPMR(P<0.05),术后随访中UEMR组复发率明显低于EPMR组(P<0.05)。
6药物因素
胰岛素抵抗被认为是影响腺瘤复发的关键机制[28-29]。二甲双胍可提高脂肪组织对胰岛素的敏感性及利用率、改善胰岛素抵抗、激活AMPK及抑制mTOR通路抑制肿瘤发生和癌细胞生长[30]。Higurashi T等[31]前瞻性研究显示,二甲双胍可预防非糖尿病患者息肉切除术后异时性增生性息肉和腺瘤,并且低剂量二甲双胍1年的摄入对于非糖尿病患者是安全的;二甲双胍可降低糖尿病患者结肠腺瘤复发风险(P=0.001)[32]。Noreen等[33]发现定期服用阿司匹林会通过稳定DNA甲基化来控制癌症关键通路的基因。Ishikawa等[34-35]认为阿司匹林对于非吸烟者腺瘤复发具有保护作用,对于大量吸烟者其保护作用丧失。基于阿司匹林作用机制的研究可能成为未来精准药物治疗的方法[36]。
7体脂状态
体重指数(BMI,Body mass index)作为肥胖的常用衡量指标与复发性腺瘤存在正相关[37,38];内脏脂肪组织(VAT,Visceral adipose tissue)为除脊柱及椎旁肌肉以外,由腹膜壁及腹横筋膜包裹的腹腔内脂肪组织[39]。Jong Pil Im等[40]认为BMI及腰围的增加与结肠腺瘤复发风险有关,复发性结肠腺瘤VAT基线面积明显高于未复发结肠腺瘤者;kim等[38]随访发现,VAT基线面积与腺瘤的复发及生长有关,其相对于BMI、腰围对结肠腺瘤的预测价值更高;Jihye Park等[41]认为晚期腺瘤复发独立危险因素为体脂质量和积极运动,美国癌症协会结肠癌生存护理指南及韩国癌症中心建议,每周至少锻炼150分钟以保持健康体重[42]。
8其他
年龄是腺瘤复发的危险因素[4,17,39];男性、肠道准备不足更容易发生复发高危息肉[15,39],美国息肉切除术后监测指南指出男性患高危息肉风险较高,肠道准备不足者应在1年内复查结肠镜[7]。
9展望
结肠息肉切除术后监测是结直肠癌预防策略之一,目前结肠息肉切除术后随访指南多根据肠镜镜检结果指[1,6,7],缺乏个体化且亚组分型不明,监测过少可能达不到结肠癌预防目标,过频可能造成结肠镜低效利用[43,44]。结肠息肉复发预测的研究仍在进行:Mayenaaz等[45,46]通过大小/形态/位置/通路(SMSA,The size/morphology/site/access)息肉评分系统评估认为SMSA4可作为复发腺瘤的预测因子(P<0.05);Linda Brand等[47]认为β-catenin、cox-2表达与腺瘤复发显著相关(P<0.01);目前对于结肠息肉复发相关研究有限,今后有必要进行大规模研究以指导个体化结肠息肉术后监测时间的制定,为结肠息肉术后复发的预测及预防提供依据。
参考文献
[1]Nishihara R,Wu K,Lochhead P et al.Long-term colorectal-cancer incidence and mortality after lower endoscopy[J].N Engl J Med,2013,369(12):1095-1105.
[2]Atkin W,Wooldrage K,Parkin DM,et al.Long term effects of once-only flexible sigmoidoscopy screening after 17 years of follow-up:the UK Flexible Sigmoidoscopy Screening randomised controlled trial[J].Lancet,2017,389(10076):1299-1311.
[3]HolmeØ,Løberg M,Kalarer M,et al.Long-Term Effectiveness of Sigmoidoscopy Screening on Colorectal Cancer Incidence and Mortality in Women and Men:A Randomized Trial[J].Ann Intern Med,2018,169(9):663-664.
[4]Choi WS,Han DS,Eun CS et al.Three-year colonoscopy surveillance after polypectomy in Korea:a Korean Association for the Study of Intestinal Diseases(KASID)multicenter prospective study[J].Intest Res 2018,16(1):126-133.
[5]Cubiella J,Arias MD,Penin MC.Immunohistochemical alterations in invasive adenocarcinoma in endoscopically resected adenoma and factors associated with risk of residual or recurrent disease[J].Colorectal Dis,2012,14(9):e587-594.
[6]Bogie R,Sanduleanu S.Optimizing post-polypectomy surveillance:a practical guide for the endoscopist[J].Dig Endosc,2016,28(3):348-359.
[7]Lieberman DA,Rex DK,Winawer SJ,et al.Guidelines for colonoscopy surveillance after screening and polpectomy:a consensus update by the US Multi-Society Task Force on Colorectal Cancer[J].Gastroenterology,2012,143(3):844-857.
[8]Briedigkeit A,Sultanie O,Sido B,et al.Endoscopic mucosal resection of colorectal adenomas>20 mm:Risk factors for recurrence.World J Gastrointest Endosc,2016,10(8):276-281.
[9]Tate DJ,Desomer L,Klein A,et al.Adenoma recurrence after piecemeal colonic EMR is predictable:the Sydney EMR recurrence tool[J].Gastrointest Endosc,2017,85(3):647-656.
[10]Facciorusso A,Di Maso,Serviddio G,et al.Factors associated with recurrence of advanced colorectal adenoma after endoscopic resection[J].Clin Gastroenterol Hepatol,2016,14(8):1148-1154.
[11]Hauq U,Senore C.Long-term colorectal-cancer mortality after adenoma removal[J].N Engl J Med,2014,371(21):2035-2037.
[12]Moss A,Williams SJ,Hourigan LF,et al.Long-term adenoma recurrence following wide-field endoscopic mucosal resection(WF-EMR)for advanced colonic mucosal neoplasia is infrequent:results and risk factors in 1000 cases from the Australian Colonic EMR(ACE)study[J].Gut,2015,64(1):57-65.
[13]Oka S,Tanaka S,Saito Y,et al.Local recurrence after endoscopic resection for large colorectal neoplasia:a multicenter prospective study in Japan[J].Am J Gastroenterol,2015,110(5):697-707.
[14]Pohl H,Srivastava A,Bensen SP,et al.Incomplete polyp resection during colonoscopy-results of the complete adenoma resection(CARE)study[J].Gastroenterology,2013,144(1):74-80.
[15]Janq HW,Park SJ,Hong SP,et al.Risk Factors for Recurrent High-Risk Polyps after the Removal of High-Risk Polyps at Initial Colonoscopy[J]. Yonsei Med J,2015,56(6):1559-1565
[16]Vleugels JLA,Hassan C,Senore C,et al.Diminutive Polyps With Advanced Histologic Features Do Not Increase Risk for Metachronous Advanced Colon Neoplasia[J].Gastroenterology,2019,156(3):623-634.
[17]Pommergaard HC,Burcharth J,Rosenberg J,et al.Advanced age is a risk factor for proximal adenoma recurrence following colonoscopy andpolypectomy[J].Br J Surq,2016,103(2):e100-105.
[18]Beg S,Siraj AK,Prabhakaran S,et al.Molecular markers and pathway analysis of colorectal carcinoma in the Middle East[J].Cancer,2015,121(21):3799-3808.
[19]Dumoulin FL,Hildenbrand R.Endoscopic resection techniques for colorectal neoplasia:Current developments[J].World J Gastroenterol,2019,25(3):300-307.
[20]Belderbos TD,Leenders M,Moons LM,Siersema PD.Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions:systematic review and meta-analysis[J].Endoscopy,2014,46(5):388-402.
[21]Knabe M,Pohl J,Gerges C,et al.Standardized long-term follow-up after endoscopic resection of large,nonpedunculated colorectal lesions:a prospective two-center study[J].Am J Gastroenterol,2014,109(2):183-189.
[22]Itos S,Hotta K,Imai k,et al.Treatment strategy for local recurrences after endoscopic resection of a coloerectal neoplasm[J].Surq Endosc,2019,33(4):1140-1146.
[23]Bahin FF,Heitman SJ,Bourke MJ,et al.Wide-field endoscopic mucosal resection versus endoscopic submucosal dissection for laterally spreading colorectal lesions:a cost-effectiveness analysis[J].Gut,2018,67(11):1965-1973.
[24]Arezzo A,Passera R,Marchese,et al.Systematic review and meta-analysis of endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal lesions[J].United European Gastroenterol J,2016,4(1):18-29.
[25]Tanka S,Kashida H,Saito Y,et al.JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection[J].Dig Endosc,2015,27(4):417-434.
[26]Schenck RJ,Jahann DA,Patrie JT,et al.Underwater endoscopic mucosal resection is associated with fewer recurrences and earlier curative resections compared to conventional endoscopic mucosal resection for large colorectal[J].Surg Endosc,2017,31(10):4174-4183.
[27]Kim HG,Thosani N,Banerjee S,et al.Underwater endoscopic mucosal resection for recurrences after previous piecemeal resection of colorectal polyps(with video)[J].Gastrointest Endosc,2014,80(6):1094-1102.
[28]Viollet B,Guigas B,Sanz Garcia N,et al.Cellular and molecular mechanisms of metformin:an overview[J].Clin Sci(Lond),2012,122(6):253-270.
[29]Laiyemo AO.The risk of colonic adenomas and colonic cancer in obesity[J].Best Pract Res Clin Gastroenterol,2014,28(4):655-663.
[30]Hawley SA,Ross FA,Chevtzoff C,et al.Use of cells expressing gamma subunit variants to identify diverse mechanisms of AMPK activation[J].Cell Metab,2010,11(6):554-565.
[31]Higurashi T,Hosons K,Takahashi H,et al.Metformin for chemoprevention of metachronous colorectal adenoma or polyps in post-polypectomy patients without diabetes:a multicentre double-blind,placebo-controlled,randomised phase 3 trial[J].Lancet Oncol,2016,17(4):475-483.
[32]Han MS,Lee HJ,Park SJ,et al.The effect of metformin on the recurrence of colorectal adenoma in diabetic patients with previous colorectal adenoma[J].Int J colorectal Dis,2017,32(8):1223-1226.
[33]Noreen F,Roosli M,Gaj P,et al.Modulation of age-and cancer-associated DNA methylation change in the healthy colon by aspirin and lifestyle[J].J Natl Cancer Inst,2014,106(7):duj 161.
[34]Ishikawa H,Mutoh M,Suzuki S,et al.The preventive effects of low-dose enteric-coated aspirin tablets on the development of colorectal tumours in Asian patients:a randomised trial[J].Gut,2016,63(11):1755-1759.
[35]David DA,Goh G,Mo A,et al.Colorectal polyp prevention by daily aspirin use is abrogated among active smokers[J].Cancer Causes Control,2016,27(1):93-103.
[36]McFerran E,O'Mahony JF,Fallis R,et al.Evaluation of the Effectiveness and Cost-Effectiveness of Personalized Surveillance After Colorectal Adenomatous Polypectomy[J].Epidemiologic Rev,2017,39(1):148-160.
[37]Ben Q,An W,Jiang Y,et al.Body Mass Index Increases Risk for Colorectal Adenomas Based on Meta-analysis[J].Gastroenterology,2012,142(4):762-772.
[38]Okabayashi K,Ashrafian H,Hasegawa H,et al.Body mass index category as a risk factor for colorectal adenomas:a systematic review and meta-analysis[J].Am J Gastroenterol,2012,107(8):1175-1185.
[39]Kim B,Kim BC,Nam SY,et al.Visceral Adipose Tissue Volume and the Occurrence of Colorectal Adenoma in Follow-up Colonoscopy for Screening and Surveillance[J].Nutr Cancer,2017,69(5):739-745.
[40]JP Im,Kim D,Chung SJ,et al.Visceral obesity as a risk factor for colorectal adenoma occurrence in surveillance colonoscopy[J].Gastrointestinal Endosc,2018,88(1):119-127.
[41]Park J,Kim JH,Lee HJ,et al.The effects of physical activity and body fat mass on colorectal polyp recurrence in patients with previous colorectal cancer[J].Cancer Prev Res,2017,10(8):478-483.
[42]El-Shami K,Oeffinger KC,Erb NL,et al.American Cancer Society Colorectal Cancer Survivorship Care Guidelines[J].CA Cancer J Clin,2015,65(6):428-455.
[43]Ladabaum U,Schoen RE.Post-polypectomy surveillance that would please Goldilocks-not too much,not too little,but just right[J].Gastroenterolo gy,2016,150(4):791-796.
[44]Van Heijningen EM,Lansdorp-Vogelaar I,Steyerberg EW,et al.Adherence to surveillance guidelines after removal of colorectal adenomas:a large,community-based study[J].Gut,2015,64(10):1584-1592.
[45]Sidhu M,Tate DJ,Dsomer L,et al.The size,morphology,site,and access score predicts critical outcomes of endoscopic mucosal resection in the colon[J].Endoscopy,2018,50(7):684-692.
[46]Barosa R,Mohammed N,Rembacken B,et al.Risk stratification of colorectal polyps for predicting residual or recurring adenoma using the Size/Morphology/Site/Access score[J].United European Gastroenterology J 2018,6(4)630-638.
[47]Brand L,Munding J,Pox cp,et al.ß-catenin,Cox-2 and p53 immunostaining in colorectal adenomas to predict recurrence after endoscopic polypectomy[J].Int J Colorectal Dis,2013,28(8):1091-1098.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网! 文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/18876.html