SCI论文(www.lunwensci.com):
ABSTRACT:Objective(1)To explore the correlation between HPV genotype versus biopsy pathological diagnosis by using Fisher exact test.(2)To explore the correlation between extent of TCT cytological abnormality versus biopsy pathological diagnosis by using gamma correlation test.(3)To explore the demographic distribution of TCT-HPVpositive diagnosis among Qinghai women by their age specific prevalence.Methods This study retrospectively utilized hospital records at Qinghai Hospital,patients attending the department of obstetrics and gynecology,between April 2014 to December 2018.The exposure of interest was HPV positive diagnosis measured by TCT.For all patients that fit criteria for age(18-70years)and non-comorbid to other gynecological cancers were sorted for data collection.Their cervical screening results,HPV-genotyping and biopsy’s pathological diagnoses were recorded.HPV distribution among eligible participants was descriptively illustrated by age-specific prevalence.The correlation between extent of TCT cytological abnormality versus biopsy pathological diagnosis by using gamma correlation test.A computer software SPSS 24.0 was used.Also,the correlation between HPV genotype versus biopsy pathological diagnosis by using Fisher exact test.Results A total of 1120 patients fulfilled criteria for participation in the study(mean age of 45.43+/-5 years).HPV-16 was the most prevalent genotype,accounting for 26.70%of all the people tested,followed by HPV-58 and HPV-52,accounting for 17.50%and 17.32,Age group 21-30 accounted for highest prevalence of HPV positive detection.The correlation between extent of TCT cytological abnormality versus biopsy pathological diagnosis showed,gamma correlation test of 0.561(P<0.001).The correlation between HPV genotype versus biopsy pathological diagnosis,showed Fisher exact test of P-value<0.005.Conclusion Accounting for highest prevalence,41-50-year age-group is mostly associated with HPV-16 genotype and mostly cause cervical cancer than other HPV genotypes among Qinghai population.The correlation between cervical cytological abnormality and HPV genotyping statistically,significantly correlates with cervical biopsy’s pathological diagnoses.
KEY WORDS:Cervical screening;Human papilloma virus;Thinprep cytology test
本文引用格式:Ifrah·Abdullah,GUO Gui-lan.Relationship between the Type of Reproductive Tract HPV Infection and Cervical Lesion in Qinghai Area;a Retrospective Study[J].World Latest Medicine Information(Electronic Version),2019,19(93):7-11.
Introduction
For decades,cervical screening programs have proven to be vital in cervical cancer prevention battle[1].Reportedly,the incidence of cervical cancer has steadily been declining over the last decade[2,3].Amid other,cervical cancer accounts fourth worldwide in terms of incidence and second in the developing world.In 2018,cervical cancer had had an estimated 570,000 cases[1,4,5].The incidence of cervical cancer is relatively high in China.In China alone,the incidence is more than five times that observed in the developed world,constituting about a third of entire world cases for cervical cancer and the cases tend to be in younger than older women[5].Approximately 8.7 to 11.3 individuals per 100,000 population and up to 45.0%of patients with invasive disease die of this preventable cancer[6].
Majority of Cervical cancer cases are due to Human Papilloma Virus(HPV)infection[7].Human papillomavirus accounts for one of the commonest sexually transmitted infection in both reproductive and menopausal women worldwide.Despite disease’s adverse course,competent immunity successfully clears the infection in within a year.For that reason,not-uncommonly,the infection may persist asymptomatically[1].Being either carcinogenic or non-carcinogenic associated,a number of HPV genotypes have been identified to exist.Only to name a few,non-carcinogenic HPV strains involve,HPV 6,11,42,43 and 44,while carcinogenic HPV are HPV16,18,31,33,35,39,45,51,52,56,58,59,and 68[8,9].Over ninety percent of all confirmed cervical cancer patients,carcinogenic HPV genotypes is found to be involved.Again,morethan sixty percent of cervical dysplasia cases are found to have been associated with carcinogenic HPV strains[1,2].Other than adverse outcome for cancer,the HPV virus persistence may cause mucosal membranes-warts.Though considered benign,the warts of some strains could develop to low or high grade squamous intraepithelial lesions(LSIL/HSIL)leading to other cancers such as vulva,anus,mouth or throat.The warts could even enlarge to interfere with micturition and pregnancy[1].
HPV caused cervical cancer,different from other cancers,has a more transparent natural history,normally involving initial precancerous lesions followed by a cancerous lesion.A precancerous lesion,often begins with cervical intraepithelial neoplasia(CIN)accompanied by progressive CIN I,CIN II,and CIN III[3,10-13].It was reported that at least 25%of women with CIN 2 and 3 progress to carcinoma in situ or invasive cancer if lesions are untreated[14-16].After decades of using Pap-Smear and HPV testing as screening tools,in recent years,a new procedure,Thinprep Cytology Test(TCT)was invented[17].Technically,different from Pap-Smear test in which a scrapping spatula or brush is swept on the glass slide for microscopy,in TCT the sample is inoculated in a liquid vial which is then processed by an automated machine to prepare a glass slide for microscopy.TCT has proven superiority over ordinary Pap-Smear test in terms of improved accuracy in early detection of cervical cells abnormality,as well as being able to diagnose microorganisms infecting the cervix including HPV and other suchas fungus and bacteria[17,18].
Despite these recent technological advancements in cervical cancer screening by Thinprep Cytology Test(TCT)and HPV testing,a relevant large-scale epidemiologic data on HPV-TCT and cervical cancer has been scarce among women in Qinghai Province,in the for 10 years.
Therefore,this study was aimed to explore the age specific prevalence of TCT-HPV positive diagnosis;assess the correlation between extent of TCT cytological abnormality versus biopsy pathological diagnosis by using gamma correlation test;and assess the correlation between HPV genotype versus biopsy pathological diagnosis by using Fisher exact test among Qinghai women.
1Methods and material
1.1Dates,exposure and periods of recruitment
This study involved patients attending obstetrics and gynecology department at Qinghai Hospital as either outpatient or inpatient,between April 2014 to December 2018.The exposure of interest was HPV positive diagnosis measured by TCT and biopsy.The study had one period of recruitment in that,patients participated once in the data collection process while normal TCT and HPV positive follow-up was required every 6 month or 1 year as treatment guideline,as per this study.
1.2Data collection
This study involved retrospectively extracting data from hospitals electronic database for patients’records.Demographic data were extracted from participants’records who fit criteria for inclusion in our study.Furthermore,records of three procedures were extracted;one,Thin-layer cytology test(TCT)results,HPV genotype involved in the lesion formation and pathological diagnosis result from cervical biopsy.TCT classification results were recorded as either ASC-US,ASC-H,LSIL,HSIL,AGC or Cancer.women with contact bleeding underwent colposcopic cerv i cal mul t i-point l i v e Ex ami natio n,histo patho l o g i cal diagnosis.Pathological diagnosis was recorded as either Normal/inflammation,CIN I,CIN II,CIN III or CA.Lastly,HPV genotyping was recorded as either HPV-16,HPV-18,HPV-31,HPV-33,HPV-39,HPV-52,HPV-58 or other types.Disposable cervixThe cell harvester collects cervical exfoliated cell specimens and protects them at 4°C.Save.Experimental operation and results of HPV typing testKit instructions.
1.3TCT diagnosis
The TCT diagnostic criteria are based on the 2001(the Bethesda system,TBS)standard.According to the TCT knotThe results are divided into N/I group,ASCUS group,ASC-H group,AGC group,LSIL group andHSIL group and CA group.
1.4Sampling
Prior to sampling procedure,participants were supposed to be non-menstruating for more than 3 days;have disabled intravaginal drugs and have not had sexual intercourse within past 2 days.
Sampling technique involved,use of a cotton swab to wipe and clean secretions from vaginal and cervix.While placed on the cervical opening,the brush was rotated 5 turns clockwise,then immersed in a vial with a dedicated cell preservation solution.The vials containing specimen were stored at 4°C and run in Thinprep automated Processing machine,to prepare glass slide within one week.
1.5Statistical methods
Data was analyzed separately according to the objective of interest.Demographic distribution of TCT-HPV positive results was descriptively analyzed by their age specific prevalence.The correlation between extent of TCT cytological abnormality versus biopsy’s pathological diagnosis was done by using gamma correlation test utilizing computer software SPSS version 24.0.The correlation between HPV genotype versus biopsy pathological diagnosis by using Fisher exact test utilizing computer software SPSS version 24.0.A p-value of less than 0.05 was considered statistically significant.
2Results
2.1HPV genotypes with pathologic diagnosis
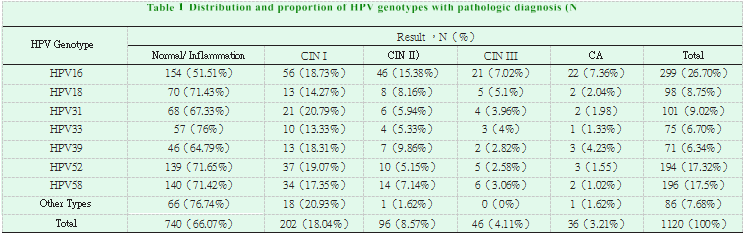
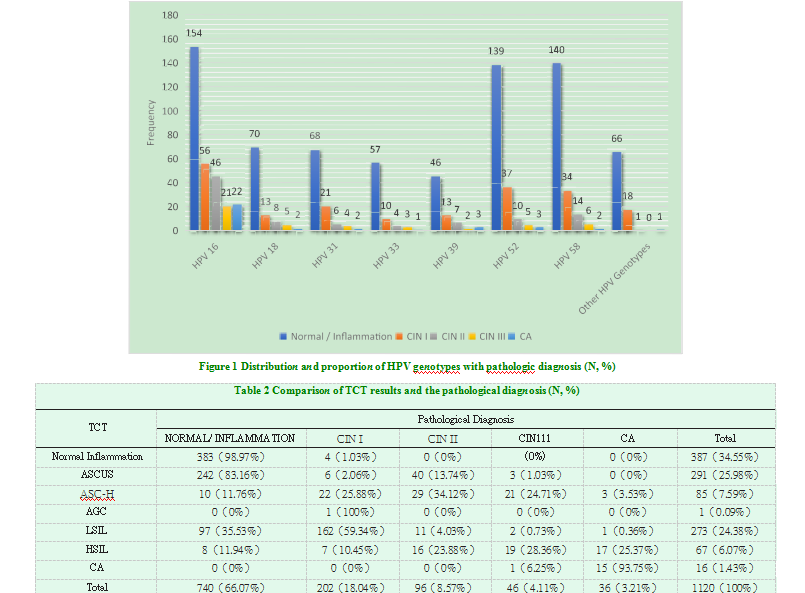
Table 1 illustrates the distribution of pathological diagnoses among different HPV genotyping results.Of all 1120 participants,those who tested for HPV16 were 299(26.70%),HPV18 were 98(8.75%),HPV31 were 101(9.02%),HPV33 were 75(6.70%),HPV39 were 71(6.34%),HPV52 were 194(17.32%),HPV58 were196(17.5%)and those who tested for Other Types were 86(7.68%).Furthermore,for those who underwent colposcopy and biopsy,740(66.07%)had Normal/inflammation;202(18.04%)with CIN I;96(8.57%)with CIN II;46(4.11%)with CIN III and 36(3.21%)withCA.These results are diagrammatically depicted by Figure 1.
2.2Statistical analysis for HPV genotypes with pathologic diagnosis
Table 1 shows among all the HPV positive patients,most patients were infected by the HPV 16(26.70%),followed by HPV-58(17.5%)and HPV52(17.32%).It indicated that in the Qinghai,China,the most prevalent HPV genotype were HPV 16,58 and 52.Within one HPV genotype,most patients were diagnosed as normal/inflammation.Fisher exact test produced a P-value of 0.000.There was significant difference between different HPV genotype and pathological diagnosis(P<0.05).HPV Genotype Result,N(%) Normal/Inflammation CIN I CIN II) CIN III CA Total HPV16 154(51.51%)56(18.73%)46(15.38%)21(7.02%)22(7.36%)299(26.70%)HPV1870(71.43%)13(14.27%)8(8.16%)5(5.1%)2(2.04%)98(8.75%)HPV3168(67.33%)21(20.79%)6(5.94%)4(3.96%)2(1.98)101(9.02%)HPV3357(76%)10(13.33%)4(5.33%)3(4%)1(1.33%)75(6.70%)HPV3946(64.79%)13(18.31%)7(9.86%)2(2.82%)3(4.23%)71(6.34%)HPV52139(71.65%)37(19.07%)10(5.15%)5(2.58%)3(1.55)194(17.32%)HPV58140(71.42%)34(17.35%)14(7.14%)6(3.06%)2(1.02%)196(17.5%)Other Types66(76.74%)18(20.93%)1(1.62%)0(0%)1(1.62%)86(7.68%)Total740(66.07%)202(18.04%)96(8.57%)46(4.11%)36(3.21%)1120(100%)
2.3TCT results and HPV testing
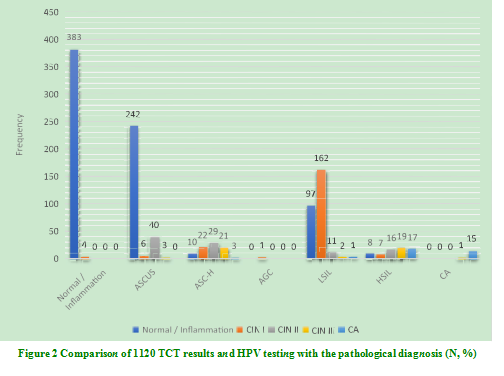
Table 2 illustrates the crosstabulation of pathological diagnoses among different TCT screening results.Of 1120 participants,387(34.55%)screened Normal/Inflammation;(25.98%)screened ASCUS;85(7.59%)screened ASC-H;1(0.09%)screened AGC;273(24.38%)screened LSIL;67(6.07%)screened HSIL and 16(1.43%)screened CA.Pathological diagnoses prevalence was highest for normal/inflammation 740(66.07%)descending through CIN I(18.04%),CIN II(8.57%),CIN III(4.11%)and lowest in CA 36(3.21%).These results are diagrammatically depicted by Figure 2.
2.4Statistical analysis of TCT cytological abnormality versus biopsy pathological diagnosis
Tabl e 2 il lustrates the correlati on between TCT and Pathological Diagnosis were conducted in subjects.In TCT,66.07%patients were found in the normal/inflammation,18.04%patients in CIN I.In the pathological diagnosis 25.98%patients were diagnosed in ASCUS,34.55%patients were normal/inflammation and 24.38%were in the LSIL.The Gamma Coefficient were 0.561(P<0.001).
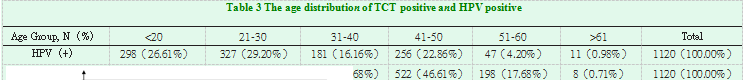
2.5Age-specific prevalence for HPV and TCT
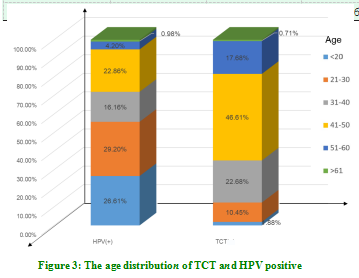
Table 3 shows the distribution of HPV positive and TCT results by age.The table also illustrates the method used for screening with both TCT and HPV rapid diagnostic test.The most prevalent HPV positive participants were 21-30 years old(29.20%)declining through<20(26.61%),41-50(22.86%),31-40 (16.16%), 51-60 (4.2%) and age group >61accounting the least with only 0.98%. TCT, on the other hand had highest frequency in the 41-50 age group ( 46.61%) declining through 31-40 (22.68%), 51-60(17.68%), 21-30 (10.45%), <20 (1.88%) while
age group >60 accounted least with only 0.71%.These results are diagrammatically depicted by Figure 3.
3Discussion
Pap-Smear and HPV testing as screening tools,for long,revolutionized cervical cancer screening leading to the significant reduction of incidences in the past thirty years.Though still in the top five cancers in the world by prevalence,cervical cancer is up to further reduction in incidences and prevalence since invention of a new procedure,Thinprep Cytology Test(TCT).Technically,TCT is different from Pap-Smear test in which a scrapping spatula or brush is swept on the glass slide for microscopy[19].In TCT the cervical scrap sample is inoculated in a liquid vial which is then processed by an automated machine to prepare a glass slide for microscopy.TCT has proven superiority over ordinary Pap-Smear test in terms of improved accuracy in early detection of cervical cells abnormality,as well as being able to diagnose microorganisms infecting the cervix including HPV and other such as fungus and bacteria[17,18,20].
Despite these recent technological advancements in cervical cancer screening by Thinprep Cytology Test(TCT)over an ordinary Pap-smear test[21],little is known about how the advancement affected the epidemiology of the cancer among women in Qinghai province.Therefore,this study was to explore the demographic age specific prevalence of TCT-HPV positive diagnosis;assess the correlation between extent of TCT cytological abnormality versus biopsy pathological diagnosis by using gamma correlation test;and assess the correlation between HPV genotype versus biopsy pathological diagnosis by using Fisher exact test among Qinghai women.
From a total of 1120 patients who fulfilled criteria for participation in our study(mean age of 45.43+/-5 years)all were tested by TCT.HPV-16 was found to be the most prevalent genotype,accounting for 26.70%,of all the people tested,followed by HPV-58 and HPV-52,accounting for 17.5%and 17.32%,respectively while HPV-39,accounted for the lowest,6.34%%.Pathological diagnoses prevalence was highest for normal/inflammation 740(66.07%)descending through CIN I(18.04%),CIN II(8.57%),CIN III(4.11%)and lowest in CA 36(3.21%).Cervical screening results showed Normal/Inflammation 383(98.97%)with highest proportions descending through ASCUS(25.98%),LSIL(24.38%),ASC-H(7.59%),HSIL (6.07%),CA(1.43%)and ACG(0.09%)The most prevalent HPV positive participants were 21-30 years old(29.20%)declining through<20(26.61%),41-50(22.86%),31-40(16.16%),51-60 (4.2%)and age group>61accounting the least with only 0.98%.TCT,on the other hand had highest frequency in the 41-50 age group(46.61%)declining through 31-40(22.68%),51-60(17.68%),21-30(10.45%),<20(1.88%)while age group>60 accounted least with only 0.71%.The correlation between extent of TCT cytological abnormality versus biopsy pathological diagnosis showed,gam ma correlation test of 0.561(P<0.001).T he correlation between HPV genotype versus biopsy pathological diagnosis,showed Fisher exact test of P-value<0.005.
The conclusion for this study aligns with several other studies,though participants with different demographics were utilized[22-28].In England,Howell-Jones et al.(2010)[22]demonstrated that women of all ages undergoing screening,the prevalence of HPV 16 and/or 18 was 15.7%(95%CI 11.2-21.6%)and 5.1%(95%CI 3.3-8.0%),respectively.Furthermore,the prevalence of HPV 16 and/or 18 increased with increasing severity of cytology grade,and was higher among younger women,within all cytology grades(more markedly in the lower grades).Chido-Amaduoyi et al.(2019)[23]demonstrated in the United States,as age increased,the weighted prevalence of abnormal cervical cancer screening outcomes decreased.Krings et al.(2019)[26]in their work further illustrated in the United States that,the five most common detected HPV types were HPV16(7.4%;95%CI:6.3-8.7),HPV52(7.2%;95%CI:6.1-8.5),HPV35(4.8%;95%CI:3.9-5.8),HPV59(4.7%;95%CI:3.8-5.8),HPV56(3.9%;95%CI:3.1-4.8).Highest prevalence was observed among women aged 18-24 years,while age 25-54 years was inversely associated with high risk HPV positivity.
Furthermore,despite statistical insignificance observed by age groups for abnormal cytology tests(chi-square p=0.67),Ilsiu et al.(2019)[25]demonstrated in Romania population that the age-standardized prevalence of HPV was 16.9%(95%CI:14.7-19.5%).For age-specific prevalence,HPV infection was found to be the highest in the age groups of women younger than 34 years old(99;23.1%HPV positive;chi-square p<0.001).In Uganda,as demonstrated by Nakalembe et al.(2019)[27],the prevalence of any HPV E6/E7 mRNA in vaginal samples was high,but the prevalence of the most oncogenic HPV types(16,18,or 45)was substantially lower.On the other hand,it worth to note that Qinghai population,by far,shares epidemiological distribution of HPV-infection with worldwide reported ones.
4Conclusion
Accounting for highest prevalence,41-50-year age-group is mostly associated with HPV-16 genotype and mostly cause cervical cancer than other HPV genotypes among Qinghai population.The correlation between cervical cytological abnormality and HPV genotyping statistically,significantly correlates with cervical biopsy’s pathological diagnoses.
References
[1]Tao,X.,et al.Follow-up with histopathology and HPV testing on LSIL cytology in China’s largest academic woman’s hospital[J].Cancer Cytopathology,2019,127(4):258-266.
[2]Sreedevi,A.,R.Javed,A.Dinesh.Epidemiology of cervical cancer with special focus on India[J].International journal of women’s health,2015,7:405-414.
[3]Markowitz,L.E.,et al.Declines in HPV vaccine type prevalence in women screened for cervical cancer in the United States:Evidence of direct and herd effects of vaccination[J].Vaccine,2019,37(29):3918-3924.
[4]Brebi,P.,et al.Frequency of Human papillomavirus in women attending cervical cancer screening program in Chile[J].BMC Cancer,2017,17(1):518.
[5]Zeng,X.-X.,et al.Prevalence and genotype distribution of human papillomavirus among Hakka women in China[J].Annals of translational medicine,2016,4(15):276-276.
[6]Tsedenbal,B.,et al.Human papillomavirus genotyping among women with cervical abnormalities in Ulaanbaatar,Mongolia[J].International Journal of Infectious Diseases,2018,77:8-13.
[7]Sousa,H.,et al.High-Risk human papillomavirus genotype distribution in the Northern region of Portugal:Data from regional cervical cancer screening program[J].Papillomavirus Res,2019:100179.
[8]Wang,Y.,et al.Genotype Distribution of Human Papillomavirus among Women with Cervical Cytological Abnormalities or Invasive Squamous Cell Carcinoma in a High-Incidence Area of Esophageal Carcinoma in China[J].BioMed research international,2016:1256384-1256384.
[9]Zhang,Q.,et al.Assessment of the effectiveness of HPV16/18 infection referred for colposcopy in cervical cancer screening in Northwest of China[J].2018,90(1):165-171.
[10]Chong,G.O.,et al.Prevalence,survival outcomes,and clinicopathologic factors associated with negative high risk human papillomavirus in surgical specimens of cervical cancer with pretreatment negative DNA genotype test[J].Int J Gynecol Cancer,2019,29(1):10-16.
[11]Liao,L.,et al.Prevalence and distribution of human papillomavirus genotypes among women with high-grade squamous intraepithelial lesion and invasive cervical cancer in Ganzhou,China[J].J Clin Lab Anal,2019,33(3):e22708.
[12]Phaswana-Mafuya,N.and K.Peltzer,Breast and Cervical Cancer Screening Prevalence and Associated Factors among Women in the South African General Population[J].Asian Pac J Cancer Prev,2018,19(6):1465-1470.
[13]Snyman,L.C.,et al.Use of a Sentinel Lymph Node Biopsy Algorithm in a South African Population of Patients With Cervical Cancer and High Prevalence of Human Immunodeficiency Virus Infection[J].Int J Gynecol Cancer,2018,28(7):1432-1437.
[14]Del Mistro,A.,et al.Long-Term Clinical Outcome after Treatment for High-Grade Cervical Lesions:A Retrospective Monoinstitutional Cohort Study%J BioMed Research International[J].2015:8.
[15]Wang,J.-L.,et al.Application of Human Papillomavirus in Screening for Cervical Cancer and Precancerous Lesions[J].Asian Pacific journal of cancer prevention:APJCP,2013,14:2979-2982.
[16]Zhang,Q.,et al.Epidemiological Investigation and Risk Factors for Cervical Lesions:Cervical Cancer Screening Among Women in Rural Areas of Henan Province China[J].Medical science monitor:international medical journal of experimental and clinical research,2016,22:1858-1865.
[17]Wei,Y.,Y.Lu,and c.li,Clinical Application of Ultrasound-Guided Thyroid Fine Needle Aspiration Biopsy and Thinprep Cytology Test in Diagnosis of Thyroid Disease[J].Asian Pacific journal of cancer prevention:APJCP,2016,17(10):4689-4692.
[18]Huang,Y.-N.,et al.Development of Whole Slide Imaging on Smartphones and Evaluation With ThinPrep Cytology Test Samples:Follow-Up Study[J].JMIR mHealth and uHealth,2018,6(4):e82-e82.
[19]Liu,Y.,et al.The clinical research of Thinprep Cytology Test(TCT)combined with HPV-DNA detection in screening cervical cancer[J].Cell Mol Biol(Noisy-le-grand),2017,63(2):92-95.
[20]Nam,J.-H.,et al.A case of large cell neuroendocrine carcinoma of the uterine cervix misdiagnosed as adenocarcinoma in Thinprep cytology test[J].CytoJournal,2017,14:28-28.
[21]Liang,H.,et al.Evaluation of 3D-CPA,HR-HPV,and TCT joint detection on cervical disease screening[J].Oncology letters,2016,12(2):887-892.
[22]Howell-Jones,R.,et al.Multi-site study of HPV type-specific prevalence in women with cervical cancer,intraepithelial neoplasia and normal cytology,in England[J].British Journal of Cancer,2010,103(6):928-928.
[23]Chido-Amajuoyi,O.G.and S.Shete.Prevalence of abnormal cervical cancer screening outcomes among screening-compliant women in the United States[J].Am J Obstet Gynecol,2019,221(1):75-77.
[24]Fokom Domgue,J.,et al.Prevalence and determinants of cervical cancer screening with a combination of cytology and human papillomavirus testing[J].Ann Epidemiol,2019.
[25]Ilisiu,M.B.,et al.HPV Testing for Cervical Cancer in Romania:High-Risk HPV Prevalence among Ethnic Subpopulations and Regions[J].Ann Glob Health,2019,85(1).
[26]Krings,A.,et al.Characterization of Human Papillomavirus prevalence and risk factors to guide cervical cancer screening in the North Tongu District,Ghana[J].PLoS One,2019,14(6):e0218762.
[27]Nakalembe,M.,et al.Prevalence,correlates,and predictive value of high-risk human papillomavirus mRNA detection in a community-based cervical cancer screening program in western Uganda[J].Infect Agent Cancer,2019,14:14.
[29]Suteu,O.,et al.Prevalence of positive screening test results and agreement between cytology and human papillomavirus testing in primary cervical cancer screening in North-Western Romania[J].Eur J Cancer Prev,2019.
关注SCI论文创作发表,寻求SCI论文修改润色、SCI论文代发表等服务支撑,请锁定SCI论文网!
文章出自SCI论文网转载请注明出处:https://www.lunwensci.com/yixuelunwen/23166.html